I. Introduction
Odontogenic sources have been reported to contribute to approximately 10% of all cases of maxillary sinusitis [
1]. Periodontal disease, periapical pathology, unsuccessful endodontic treatment, pulp necrosis, impacted maxillary teeth, and iatrogenic factors such as tooth extraction, implant surgery, and bone grafting in the maxillary sinus can be considered as causative factors for odontogenic maxillary sinusitis [
1]. The current incidence is now estimated to be as high as 30% [
2]. Furthermore, due to advancements in sinus augmentation techniques and implantology, dental implants is the most common etiology of odontogenic sinusitis [
3].
For acute maxillary sinusitis(lasting less than 4 weeks) caused by dental implants, only the causative implant needs to be removed. However, since maxillary sinusitis caused by dental implants is mainly unilateral and progresses chronically(lasting more than 12 weeks), it is necessary to treat not only the causative implant factor but also to manage the obstructed maxillary ostium [
4,
5]. Therefore, the treatment for dental implant-related maxillary sinusitis involves removing the dental implant and infected bone graft material, and surgically managing the maxillary ostiums [
6]. Concomitant endoscopic sinus surgery(ESS) to achieve patency of the maxillary ostium is considered necessary for complete resolution of the disease, prevention of recurrence, and avoidance of complications [
7]. Some studies suggest that clinicians should prioritize removing the source of dental infection and only consider ESS if symptoms persist or if complete blockage of the ostium is observed [
8]. However, because dental implant-related sinusitis tends to become chronic for more than 12 weeks and the maxillary ostium is frequently blocked, the treatment typically involves ESS. ESS itself is a risky procedure that can lead to fatal complications, such as orbital hemorrhage and cerebrospinal fluid leakage [
9]. Moreover, it is a difficult procedure that requires general anesthesia or hospitalization [
6].
This study presents case series of patients with chronic maxillary sinusitis caused by dental implants. We aim to propose a novel approach for treatment of dental implant-related chronic maxillary sinusitis in patients with ostium obstruction. This approach involves removing the dental infection and intentionally creating an intentional oroantral fistula(OAF) without the need for ESS. Additionally, this study presents two specific exceptional cases that were not resolved using the method mentioned above.
III. Discussion
Odontogenic maxillary sinusitis is a common subtype of sinusitis, and its incidence rate has been increasing due to the widespread use of dental implants and sinus augmentation techniques [
2]. A specific protocol for the management of odontogenic maxillary sinusitis has not yet been established, but its surgical treatment options can be divided into two parts: management of dental infection and sinus surgery for patency of the maxillary ostium [
10]. Odontogenic maxillary sinusitis usually presents as chronic maxillary sinusitis of more than 12 weeks duration, usually unilaterally in the maxillary sinus with an odontogenic etiology. Therefore, the treatment should also be performed as a form of treatment for chronic maxillary sinusitis. Numerous studies have supported dental treatment combined with ESS as the most effective approach for achieving complete resolution preventing recurrences in chronic odontogenic maxillary sinusitis [
3,
6,
10]. Some studies have advocated that in cases where there is a clear dental infection source, it is logical to target the infection source first and then perform sinus surgery, such as ESS, as the next step in treatment only if symptoms persist [
7]. However, if the osteomeatal complex is obstructed, odontogenic sinusitis does not easily resolve by removal of dental infection alone, and it can be a predictor of indication for ESS [
7,
11].
Dental implant-related maxillary sinusitis is a type of odontogenic maxillary sinusitis that presents unilaterally and chronically [
4]. Causes of maxillary sinusitis following dental implant placement include perforation of the Schneiderian membrane during surgery and the presence of preexisting maxillary sinusitis [
12]. Perforation of the Schneiderian membrane leads to dislodgement of bone graft materials and contamination of the exposed implant surface inside the maxillary sinus, resulting in maxillary sinusitis [
13]. Therefore, the treatment consists of removal of both the contaminated implant and the bone graft materials [
14]. In addition, in chronic cases, the maxillary ostium may become obstructed, and sinus surgery should be performed to open the ostium at the same time [
3].
In this case series, the implant was exposed within the maxillary sinus, and despite bone grafting, the bone graft material was not clearly radiographically visible. The contaminated implant was removed, and an OAF was created with the removed portion to relieve pressure within the maxillary sinus and allow for drainage of pus and contaminants. In all patients, when the OAF was created for the first time, there was no evidence of ostium patency or fluid running through the nose when irrigated with the saline. However, after antibiotics administration and dressing, the patients showed signs indicative of the ostium patency. Then, CBCT was taken to confirm radiologic patency of the ostium, and the drain was subsequently removed. Afterwards, the OAF was closed spontaneously, or fistula closure surgery was performed using a buccal advancement flap under local anesthesia.
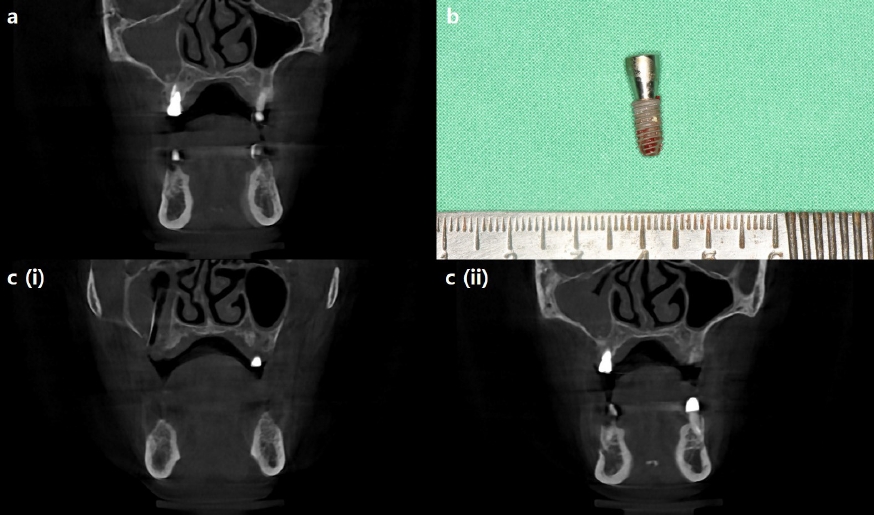
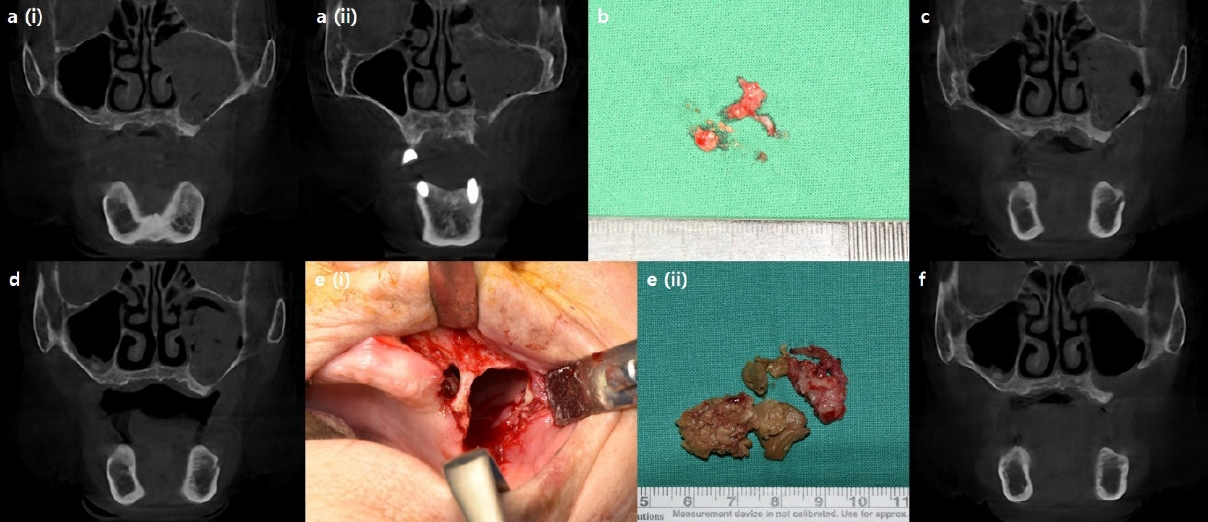
In the first three cases presented in this study, all of the maxillary sinuses exhibited severe mucosal thickening and obstructed ostium. Instead of referring patients to an ENT specialist for ESS, the dental infection sources were eliminated, and intentional OAFs were created using Penrose drains. In cases 1 and 2, the dental implants, which were the source of infection, were removed through surgical procedures. Penrose drains were then inserted through the surgical sites. In both cases, the drains were removed since dramatic decrease in mucosal thickening was observed, and ostium patency was confirmed three weeks and two weeks after the surgery.
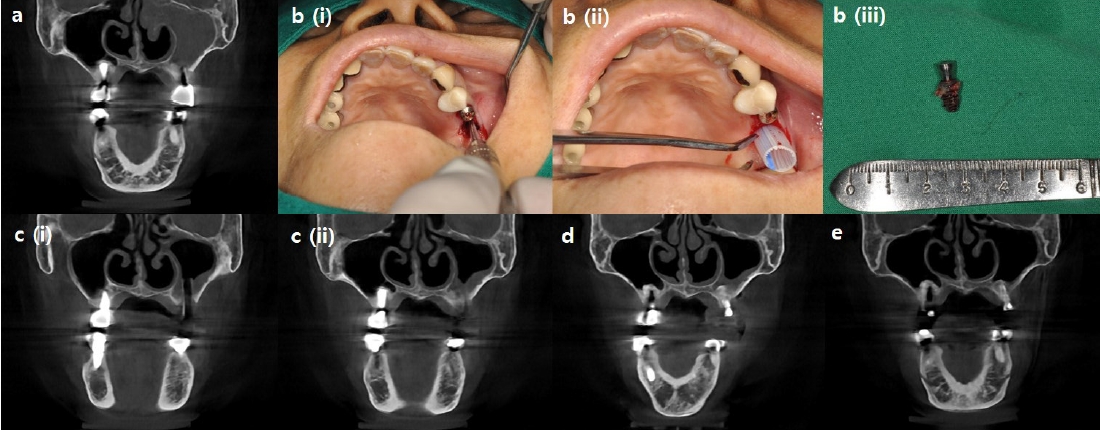
In case 3, however, the patient had already removed one of the dental implants and presented with pre-implant site gingival healing with a fully blocked ostium. Gingival incision and Penrose drain insertion was performed for creation of the intentional OAF. On the 2nd postoperative week, despite the continued obstruction of the ostium, there was a significant decrease in mucosal thickening in the right maxillary sinus, leading to the removal of the Penrose drain. On the 6th postoperative week, cleared ostium patency was finally observed. In this case, although the contaminated implant was removed beforehand, the contaminants in the maxillary sinus were not completely removed, therefore resulting in persistent chronic maxillary sinusitis. This case illustrates that chronic implant maxillary sinusitis requires treatment of the maxillary sinusitis itself as well as removal of the source of contamination.
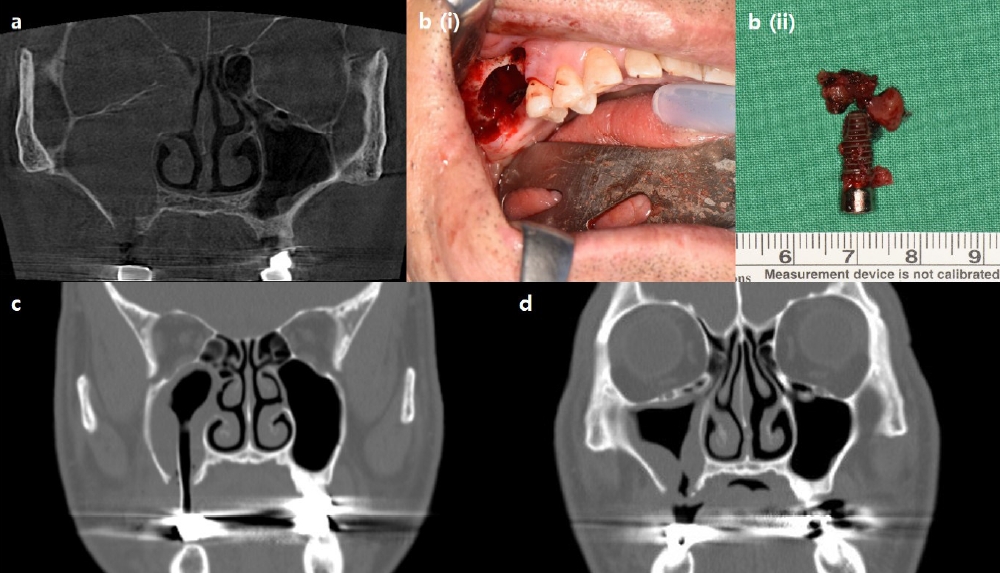
However, there were two cases in which this method did not show significant improvement in symptoms because of differences between the initial diagnosis and the final diagnosis determined by histopathological examination. In the first exception case, the patient was initially diagnosed with right maxillary sinusitis caused by the #16 implant fixture and bone graft materials. However, the final biopsy result revealed “Malignant lymphoma, suspicious for diffuse large B-cell lymphoma,” and the patient was referred to the hemato-oncology department for chemotherapy. Since diffuse large B-cell lymphoma originating from the maxillary sinus can be misdiagnosed as a benign inflammatory condition, it is important to raise awareness and explore other potential causes if the patient does not show improvement with antibiotics and standard conservative treatments [
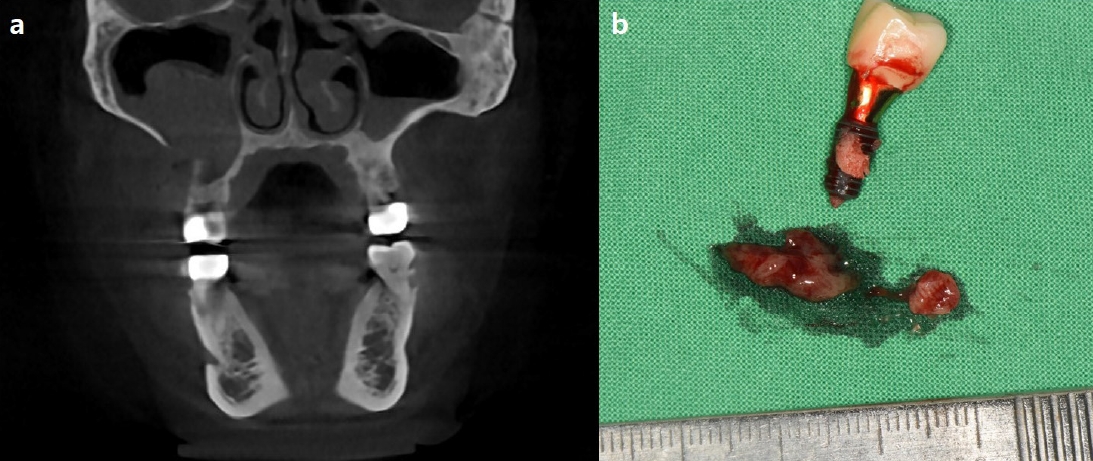
15]. In the second case, the patient was initially diagnosed with left maxillary sinusitis caused by osteomyelitis. Even after several weeks of drainage through the intentionally created oroantral fistula and antibiotic therapy, the haziness of the maxillary sinus did not seem to decrease. Therefore, other etiologies, such as fungal infections like aspergillosis, were taken into consideration and final biopsy result also confirmed the presence of aspergillosis. Since surgical debridement is the primary treatment for aspergillosis [
16], the patient underwent a surgical intervention under general anesthesia and recovered well.
As shown in these cases, when there are no signs of spontaneous ostium patency despite the treatment of chronic maxillary sinusitis as described above, or when the radiopacity of the maxillary sinus does not resolve over a prolonged period of time even if there are clinical signs of ostium patency, causes other than odontogenic origin should be suspected, such as malignancy, hematologic tumor or mycosis.
Although a gold standard for the treatment of dental implant-related chronic maxillary sinusitis has not been established, a combination of infected implant removal and ESS is widely used due to its effectiveness. However, this treatment method requires additional visits to the ENT and possibly general anesthesia and hospitalization for ESS. This study presents three cases in which patient with severe maxillary sinusitis and a blocked ostium was treated without performing ESS. The treatment involved removing the dental infection source and creating an intentional oroantral fistula by inserting a Penrose drain in the maxillary sinus. This study demonstrated that intentional oroantral communication facilitate the drainage of inflammatory tissue and the clearance of ostium obstruction in cases of maxillary sinusitis, with the exception of rare conditions such as malignant tumors or fungal infections. While this method is not universally applicable and has some limitations, it can be considered as one of the treatment options for severe odontogenic maxillary sinusitis. It can help alleviate the patient’s symptoms without the need for additional sinus surgery by an ENT specialist.







 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


