Long-term tooth preservation through supportive periodontal therapy: Report of 2 cases
Article information
Abstract
This report presents two cases demonstrating long-term tooth preservation through supportive periodontal therapy (SPT) following active treatment. Case 1 involved a 44-year-old female diagnosed with generalized Stage III periodontitis in 1988, who underwent comprehensive non-surgical and surgical treatment followed by individualized SPT for 35 years, totaling 169 recall visits. Except for one molar, all teeth remained stable. Case 2, a 41-year-old female diagnosed in 2008 with generalized Stage III periodontitis and advanced bone loss, received repeated non-surgical therapy with adjunctive doxycycline, successfully delaying multiple extractions for over 10 years until selective implants were placed. Both patients showed excellent compliance and received adjunctive interventions when indicated. These cases highlight the critical role of individualized SPT in preventing recurrence, maintaining periodontal stability, and extending tooth survival in periodontally compromised patients through periodic evaluation, risk-factor control, and continuous reinforcement of oral hygiene.
Introduction
Periodontitis is a chronic inflammatory disease of the supporting tissues of the teeth, leading to progressive attachment loss and alveolar bone destruction. The primary aim of periodontal treatment is to arrest inflammation, reduce probing pocket depth, and increase clinical attachment level. Scaling and root planing (SRP) is the foundation of nonsurgical therapy, effectively removing supragingival and subgingival local factors. Systematic reviews have reported that SRP provides clinically meaningful improvements in clinical attachment level compared with no treatment, with modest additional benefits when combined with specific adjunctive therapies such as systemic sub-antimicrobial dose doxycycline, systemic antibiotics, chlorhexidine chips, or photodynamic therapy with a diode laser [1-3].
Following successful periodontal treatment, supportive periodontal therapy is essential to prevent recurrence and further tooth loss [4,5]. SPT involves regular clinical re-evaluation, professional supra- and subgingival debridement, control of risk factors, and re-treatment of recurrent sites. Long-term studies have shown that while dropout from supportive periodontal therapy is common, patients who fully or partially adhere to SPT have significantly lower rates of tooth loss compared with those who discontinue maintenance care [6]. Evidence from multiple studies has emphasized that SPT intervals should be tailored to individual risk profiles, including systemic health status [7,8], in line with the World Health Organization’s non-communicable disease prevention framework [9].
While the benefits of SPT are well-documented in cohort studies [10,11], detailed case reports covering decades of follow-up are rare.
This report presents cases of two patients with advanced periodontitis who received active periodontal treatment followed by individualized SPT, successfully preserving their teeth for up to 35 years, highlighting the importance of a well-structured maintenance program for long-term periodontal stability and function.
Case Report
This case report was reviewed by the Institutional Review Board of Seoul National University Dental Hospital (IRB No. ERI25060). It was determined to be exempt from full review, as it involved a retrospective analysis of anonymized patient data.
Case 1
A 44-year-old female first presented in 1988 to the Department of Periodontology at Seoul National University Dental Hospital with generalized gingival discomfort. The patient had undergone orthodontic treatment approximately 30 years earlier but had no other significant dental or medical history.
Comprehensive periodontal examination in 1988 revealed generalized Stage III periodontitis, with 33% of sites showing probing depth (PD) ≥4 mm. No teeth had been lost due to periodontitis at that time. Radiographic assessment demonstrated generalized horizontal alveolar bone resorption. Initial non-surgical periodontal therapy included two visits of scaling and root planing with oral hygiene instruction, followed by full-mouth periodontal surgery performed in three appointments with flap elevation and alveolar bone recontouring.
After completion of active periodontal treatments, the patient was placed on supportive periodontal therapy and has been maintained for 35 years, attending a total of 169 recall visits. During this period, further interventions were provided as indicated. In 2004, subgingival curettage under local anesthesia was performed. In December 2007, approximately 20 years after the first visit, the maxillary right second molar was extracted due to increased mobility and bite pain. Vertical bone resorption was observed up to the apex. The following year, in 2008, an implant placement with simultaneous sinus floor elevation was performed in the maxillary right second molar region. In 2013, recurrent periodontal deep pockets were treated with full-mouth open-flap debridement, and in 2015, flap surgery was performed again in the left maxillary posterior region. Guided tissue regeneration for intrabony defects was performed at the maxillary left first molar in 2022. The procedure was limited to natural teeth with periodontal pockets ≥6 mm and no mobility. It consisted of applying an inorganic bovine bone mineral (OCS-B®, NIBEC, Jincheon, Korea) and a collagen membrane (Bio-Gide®, Geistlich Pharma AG, Wolhusen, Switzerland) after comprehensive periodontal treatment, followed by suturing.
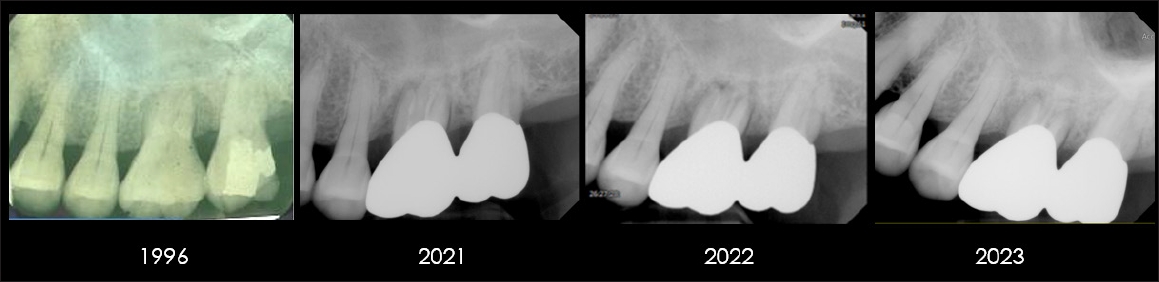
The proportion of sites with PD ≥4 mm decreased progressively over the years: 33% at baseline, 14% in 2004, 12% in 2018, and 9% in 2022 (Fig. 1). All natural teeth were preserved except for the maxillary right second molar. Serial radiographs demonstrated stable periodontal support and function throughout the 35-year follow-up period (Fig. 2).
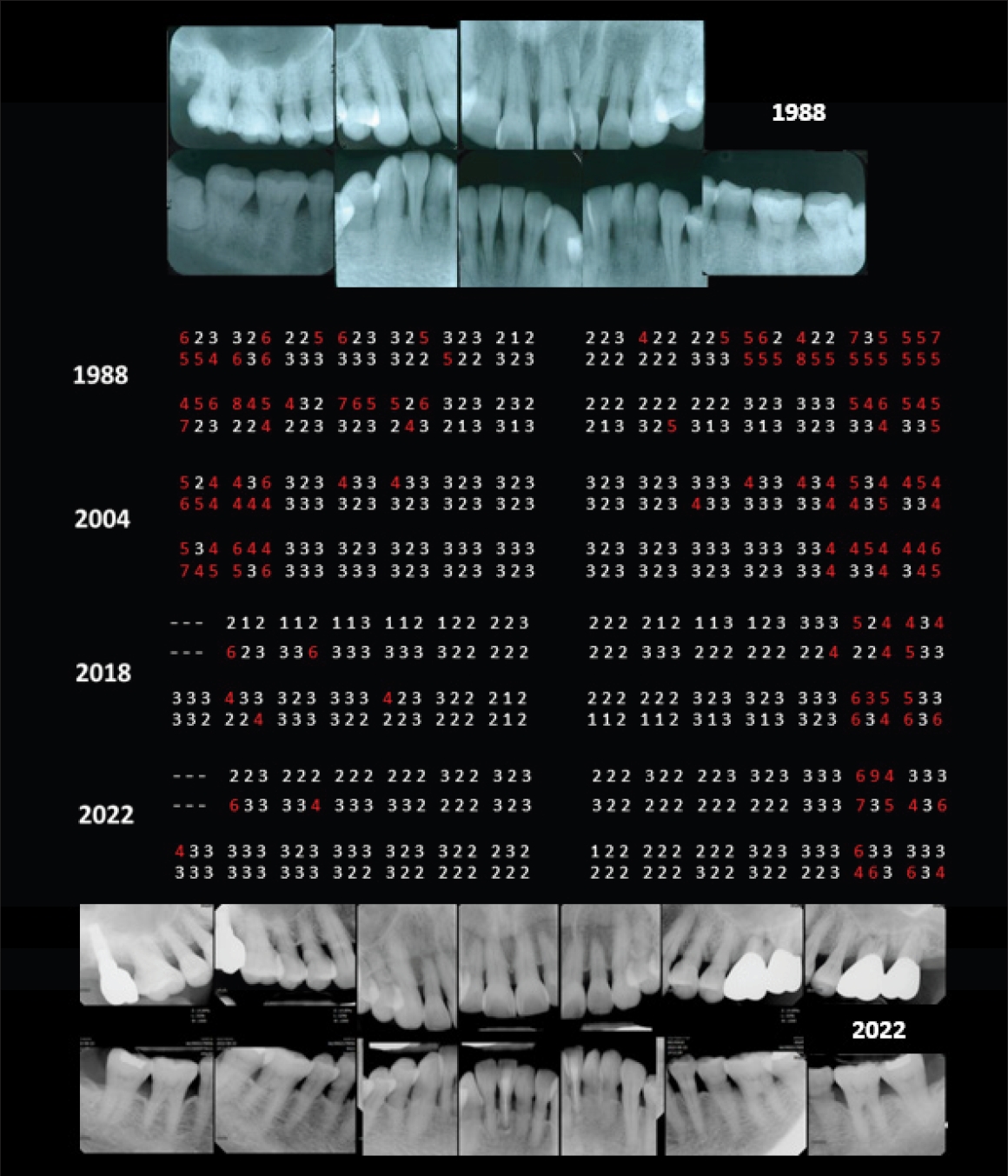
Full-mouth distribution of probing depth (PD) at four time points: baseline in 1988, and during supportive periodontal therapy at 16 years (2004), 30 years (2018), and 34 years (2022). A progressive reduction in the proportion of sites with PD ≥4 mm was observed over the 35-year maintenance period. Representative full-mouth periapical radiographs of baseline (1988) and the most recent follow-up (2022) are also presented, demonstrating generalized alveolar bone loss at initial examination and stable periodontal support after long-term maintenance.
Case 2
A 41-year-old female was referred in 2008 from the hospital for evaluation and management of generalized Stage III (severe) periodontitis. She had previously been advised of the potential need for multiple extractions and guided bone regeneration prior to implant placement. At baseline, periapical radiography revealed severe generalized alveolar bone loss and pronounced tooth mobility (Fig. 3). The patient’s medical history was non-contributory, with no evidence of systemic conditions such as diabetes or cardiovascular disease. Socially, she was employed in a stable position and reported no psychosocial factors that could interfere with treatment compliance.
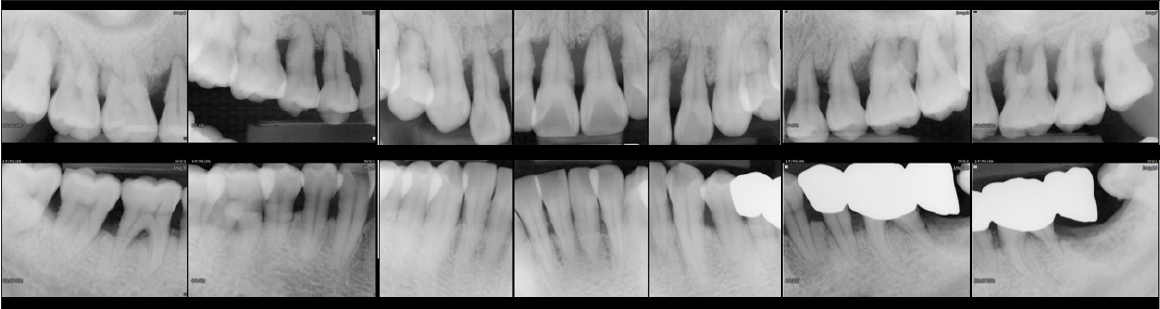
Full-mouth periapical radiograph at baseline (2008), showing generalized severe alveolar bone loss and advanced periodontal destruction
Initial non-surgical periodontal therapy consisted of two visits of SRP, supplemented with systemic doxycycline (100 mg daily for 2 weeks). At the 4-month re-evaluation, gingival recession was evident, whereas the initial findings of redness, swelling, and bleeding on probing had resolved. Radiographs demonstrated a well-defined cortical margin and stable horizontal alveolar bone levels following subgingival calculus removal (Figs. 4 and 5).

Serial periapical radiographs of the maxillary anterior region from 2008 to 2022 (year 14). Repeated non-surgical periodontal therapy contributed to relatively stable bone levels around the central incisors. Following a trauma in 2015, apex-involved bone resorption developed in the left central incisor, ultimately leading to extraction and subsequent implant placement.

Clinical photographs of the maxillary anterior region from initial presentation to post-extraction and prosthetic rehabilitation for 15 years.
At 6 months, recurrent bleeding on probing and inadequate oral hygiene control were noted. Therefore, full-mouth non-surgical therapy was repeated using meticulous ultrasonic debridement, and adjunctive doxycycline was prescribed. Thereafter, debridement was provided at 3-month intervals, performed carefully with ultrasonic instrumentation to minimize trauma to highly mobile teeth, and, in consideration of the esthetic demands in the anterior region of this young patient, flap surgery was deliberately avoided in favor of repeated and meticulous non-surgical therapy with sufficient treatment time invested.
In 2015, the maxillary left central incisor developed increased mobility following trauma during martial arts practice. A resin splint was applied for stabilization, but after 3 years, the tooth was deemed hopeless and extracted, followed by implant placement. Despite severe bone resorption at baseline, non-surgical periodontal therapy enabled the preservation of most natural teeth for more than 10 years, delaying the need for multiple extractions and prosthetic rehabilitation. This case highlights the importance of individualized decision-making in determining the appropriate timing of tooth extraction in patients with advanced periodontitis.
Discussion
The 2 cases illustrate that long-term preservation of natural dentition is possible in patients with severe periodontitis when active treatment is followed by consistent and individualized supportive periodontal therapy. Both patients were maintained on a structured recall program at approximately 3 to 6 month intervals, with comprehensive periodontal evaluation, including full-mouth probing at each visit, to detect early signs of disease recurrence. This systematic approach allowed the timely detection of attachment loss and facilitated appropriate intervention.
The optimal frequency of SPT remains debated. Classic longitudinal studies suggested that intensive prophylaxis in the early healing phase, followed by 2–6-month intervals [5,10], can effectively maintain periodontal support. More recent evidence emphasizes that recall frequency should be tailored to individual risk profiles, including residual pocket depth, bleeding on probing, systemic health, and patient compliance [11,12] In these cases, recall was scheduled every 3–6 months and adjusted according to clinical stability, reflecting a pragmatic risk-based approach.
Importantly, the favorable long-term outcomes cannot be attributed to recall frequency alone. At each maintenance visit, professional care extended beyond supragingival scaling to include meticulous subgingival debridement and thorough periodontal probing. When clinical signs such as persistent pockets ≥4 mm, bleeding on probing, or radiographic bone destruction were detected, nonsurgical re-instrumentation or surgical interventions, including open-flap debridement and regenerative therapy with guided tissue regeneration, were provided [13]. Previous studies [7,14,15] have confirmed that additional SRP during maintenance can suppress disease progression, and that its effectiveness can be enhanced when combined with re-instrumentation of deep pockets or surgical access therapy. In Case 1, the timely use of open flap debridement and regenerative treatment contributed to the stabilization of periodontal support, whereas in Case 2, repeated professional tooth cleaning with ultrasonic instrumentation helped delay tooth loss for more than a decade.
In Case 2, systemic doxycycline was used due to severe baseline bone loss and inflammatory burden. Subantimicrobial-dose doxycycline has demonstrated modest but significant benefits when combined with SRP [16], supporting its selective use in advanced cases or when surgical therapy is postponed.
Resin splinting of the maxillary incisors after trauma in 2015 provided temporary stabilization despite a poor baseline prognosis. This predictable, non-invasive interim measure allowed for the long-term maintenance of the periodontally compromised teeth until definitive treatment could be planned [17].
The long-term success of periodontal therapy largely depends on patient-performed plaque control, as professional interventions alone cannot compensate for insufficient daily oral hygiene. Previous studies demonstrated that professional reinforcement and motivation are critical to maintaining high standards of self-care [18]. Both patients in this report exhibited good compliance, which likely contributed to their favorable long-term outcomes.
Taken together, these findings align with previous evidence showing that well-structured SPT, combined with effective home care and risk-based scheduling, can maintain periodontal support for decades. They emphasize that optimal maintenance combines self-performed plaque control, individualized recall, and surgical management of recurrent disease. Nevertheless, it should be acknowledged that such favorable outcomes are not consistently achieved. The present report describes two representative cases, and the broader applicability of these findings may be limited. Patient-related factors such as compliance, systemic health status, and the initial extent of periodontal destruction remain critical determinants of long-term success.
Notes
Conflicts of Interest
None