Orbital inferior and medial wall repair via the paranasal sinus: A case report
Article information
Abstract
Orbital floor and medial wall fractures often require surgery but conventional extraoral approaches can cause scarring, eyelid malposition, and sensory changes. We report a 19-year-old male with left orbital floor, medial wall, and nasal bone fractures after a fall. The medial wall was repaired endoscopically via the ethmoid sinus, and the orbital floor was reconstructed through an intraoral transantral approach using titanium miniplates and screws. The nasal bone fracture underwent closed reduction. Postoperative CT confirmed accurate anatomical restoration. The patient achieved full recovery of ocular motility and symmetry without diplopia or enophthalmos, experiencing only transient infraorbital hypoesthesia. This case illustrates that combining intraoral transantral and endoscopic transnasal approaches provides precise, minimally invasive reconstruction for complex orbital fractures while reducing soft-tissue trauma, scarring, and postoperative complications.
Introduction
Orbital floor fractures are among the most frequent injuries resulting from blunt facial trauma and may cause functional disturbances such as diplopia, restricted ocular motility, infraorbital hypoesthesia, and delayed enophthalmos [1-3]. Surgical intervention is indicated in cases of persistent diplopia, extraocular muscle entrapment, early enophthalmos, or large bony defects [3].
Traditionally, orbital floor reconstruction has been performed through extraoral approaches such as subciliary or transconjunctival incisions [2]. These techniques provide relatively direct access to the orbital floor and facilitate placement of various reconstructive materials. However, they have inherent limitations. The subciliary approach, while offering excellent visualization of the orbital rim and floor, is frequently associated with postoperative complications including visible scarring, lower eyelid retraction, and ectropion. Conversely, the transconjunctival approach avoids an external scar but often provides limited visualization of the posterior orbital floor, particularly in cases involving large or posteriorly extended defects. In both methods, extensive dissection around the infraorbital nerve increases the risk of prolonged hypoesthesia, and manipulation of delicate periocular tissues may lead to both functional and cosmetic complications [4]. Therefore, although these conventional techniques remain effective in many cases, their drawbacks have encouraged the development of alternative approaches aimed at reducing morbidity while maintaining adequate surgical exposure.
Fractures of the medial orbital wall are also common because of its thin bony structure adjacent to the ethmoid sinus. These injuries can be difficult to detect radiographically, and inadequate reduction may lead to medial rectus muscle entrapment, horizontal gaze limitation, diplopia, and enophthalmos. Conventional external or transcaruncular approaches provide access for repair but are often associated with restricted visualization, risk of medial rectus injury, visible scarring, and postoperative morbidity [5,6].
In recent years, the management paradigm for medial orbital wall fractures has shifted toward endoscopic transnasal approaches. By accessing the ethmoid sinus under direct endoscopic visualization, surgeons can achieve precise reduction of herniated orbital contents with excellent exposure of the fracture site. This minimally invasive method avoids external incisions, minimizes soft tissue trauma, and preserves cosmetic outcomes, making it widely accepted in current clinical practice [5–9].
Similarly, the intraoral transantral approach provides distinct advantages in orbital floor reconstruction [10,11]. Through the anterior wall of the maxillary sinus, surgeons can directly visualize the defect from below, reposition herniated orbital tissue, and achieve rigid fixation using miniplates and screws [1,10,11]. This method avoids external scars and reduces periorbital tissue damage, while also allowing simultaneous management of maxillary sinus pathology if necessary [12].
When both the orbital floor and medial wall are involved, the resulting disruption of two orbital buttresses can lead to severe functional and aesthetic deformities such as marked enophthalmos and diplopia [3]. Each wall can be addressed through its respective anatomical sinus route—the orbital floor via the maxillary sinus [7,10,11] and the medial wall via the ethmoid sinus using an endoscopic approach [5–9]. This combined strategy enables targeted, minimally invasive access for complex orbital fractures, ensuring precise reduction and minimizing surgical morbidity [3,13].
The present report describes a case of successful reconstruction of combined medial and inferior orbital wall blowout fractures using an intranasal endoscopic and intraoral transantral approach, emphasizing the clinical advantages of this multidisciplinary technique.
Case Report
A 19-year-old male presented to the Emergency Department of Chonnam National University Hospital after sustaining facial trauma from slipping on the stairs. Severe swelling involving the left periorbital region and an approximately 2.0 cm laceration wound were observed on the left lower lip. The patient’s vital signs were stable, and neurological function was intact.
Clinical examination revealed normal ocular motility, intact infraorbital sensation, and well-maintained globe position without diplopia or enophthalmos.
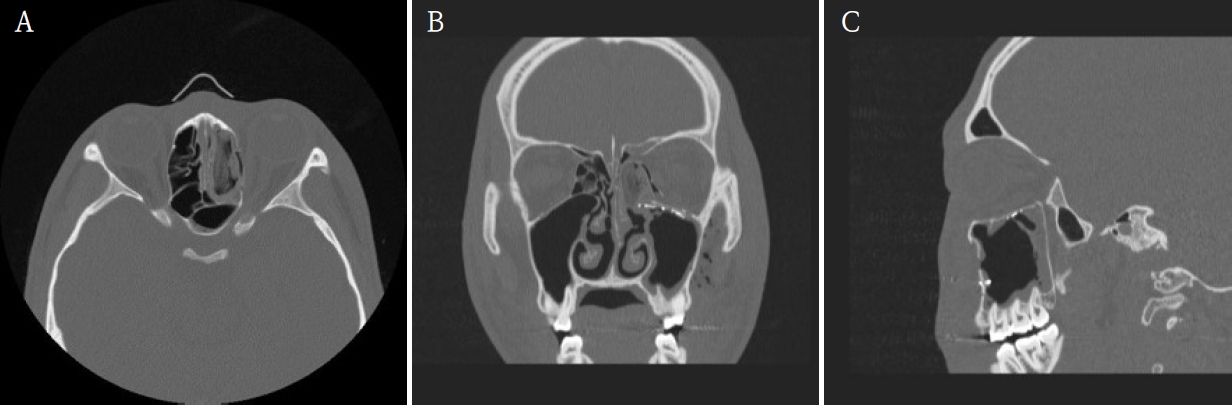
A maxillofacial CT scan was performed for further evaluation. CT imaging demonstrated fractures of the left medial orbital wall, inferior orbital wall, and nasal bone (Fig. 1). The medial wall defect was located adjacent to the ethmoid sinus with partial herniation of orbital soft tissue. The inferior orbital wall fracture extended posteriorly with minimal displacement of the bony fragments, and a depressed nasal bone fracture was also confirmed.
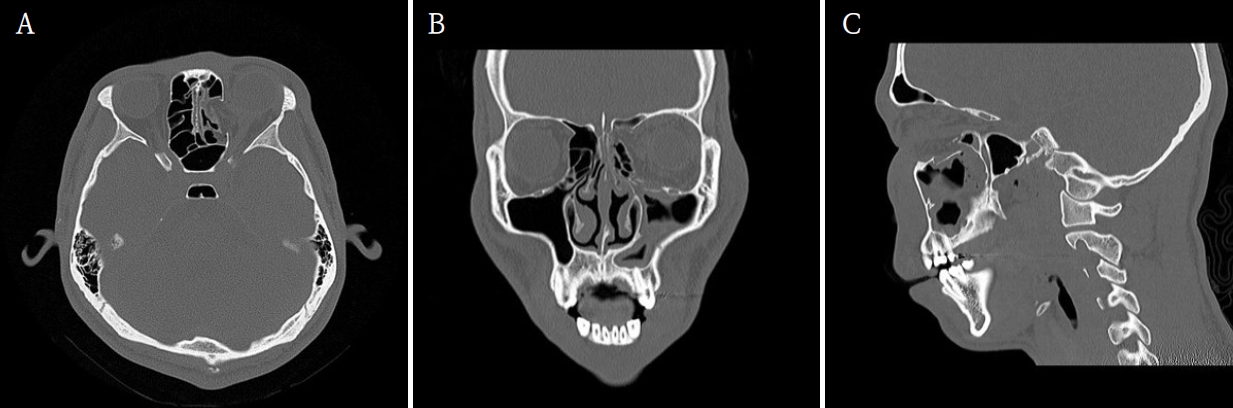
Preoperative maxillofacial computed tomographic images demonstrate the fractures of the left medial orbital wall, inferior orbital wall, and nasal bone. A. Axial view. B. Coronal view. C. Sagittal view.
Initial management included primary closure of the lower-lip laceration under local anesthesia. Reduction of the orbital and nasal bone fractures was performed under general anesthesia using a multidisciplinary approach involving the Departments of Otorhinolaryngology and Oral and Maxillofacial Surgery.
First, the medial orbital wall was repaired by the otorhinolaryngology team using an endoscopic transnasal approach with a navigation system (Fiagon Navigation System, Fiagon GmbH, Hennigsdorf, Germany). After uncinectomy and anterior ethmoidectomy, additional posterior ethmoidectomy was performed, followed by widening of the frontal and sphenoid ostia. This provided a clear surgical field for orbital compression and visualization of the left medial orbital wall fracture site (Fig. 2). The medial wall showed diffuse destruction with generalized herniation of the periorbita. After careful reduction of the herniated contents, a customized silastic sheet was inserted in an inverted U-shape (Fig. 3).
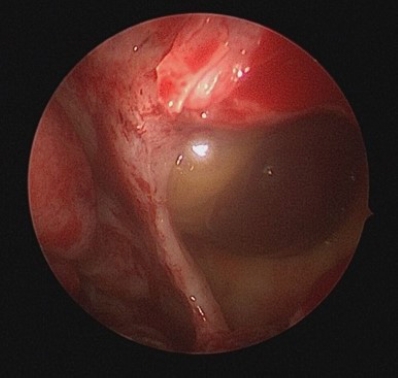
Endoscopic medial wall exposure Endoscopic view showing herniated periorbita at the medial wall defect.
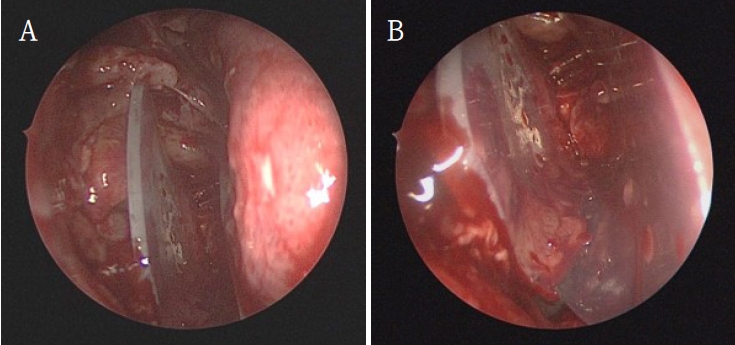
Insertion of the silastic sheet. A. Silastic sheet placement after reduction of herniated orbital tissue. B. Inverted U-shaped silastic sheet supporting the recon structed medial wall.
Subsequently, the oral and maxillofacial surgery team performed intraoral access for reconstruction of the orbital floor. A vestibular incision approximately 3 cm in length was made, extending from the left canine to the first molar region. A bony window measuring approximately 15 × 10 mm was created in the anterior wall of the maxillary sinus to provide direct visualization of the inferior orbital wall defect. Herniated orbital tissue was carefully repositioned into the orbital cavity, and the orbital floor was anatomically reconstructed. A titanium miniplate with screws (DePuy Synthes, Oberdorf, Switzerland) was applied across the fracture line to achieve rigid fixation (Fig. 4). Layered closure was then performed to ensure proper wound healing and anatomical restoration.
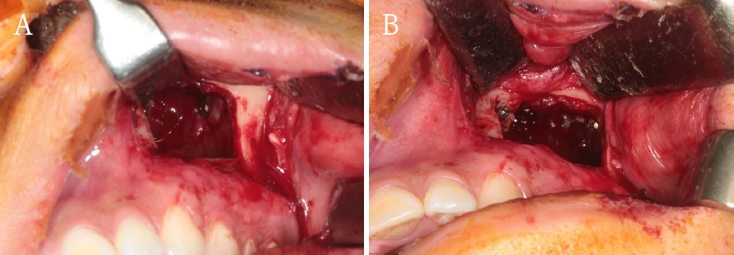
Transantral reconstruction of the inferior orbital wall. A. Intraoral transantral approach exposing the inferior orbital wall defect. B. Titanium miniplate fixation across the orbital floor fracture.
Finally, closed reduction of the nasal bone fracture was performed to restore nasal contour and symmetry. To maintain medial wall reduction and provide uniform compression, Merocel® (Medtronic Xomed, Jacksonville, FL, USA) was inserted into the ethmoid cavity. The operation proceeded smoothly without intraoperative bleeding, orbital content injury, or infraorbital nerve disturbance, indicating stable surgical control.
Immediate postoperative CT confirmed successful reduction of both fractures. The patient experienced complete resolution of diplopia and ocular discomfort, while infraorbital sensation remained mildly decreased but improving. At two weeks, Merocel® packing was removed, and routine dressing was performed. At two months, follow-up CT and endoscopic examination demonstrated stable reconstruction, and the silastic sheet was removed (Figs. 5 and 6). The patient’s sensation had nearly recovered, and postoperative outcomes remained stable with preserved ocular movement, normal globe position, and proper occlusion.
Postoperative computed tomographic (CT) images confirm successful reconstruction of the left medial and inferior orbital walls. A. Axial image shows restoration of the orbital contour with no residual herniation. B. Coronal image demonstrates stable support of the medial orbital wall and proper positioning of the orbital soft tissues. C. Sagittal image confirms an anatomically reconstructed orbital floor with maintained height and continuity.
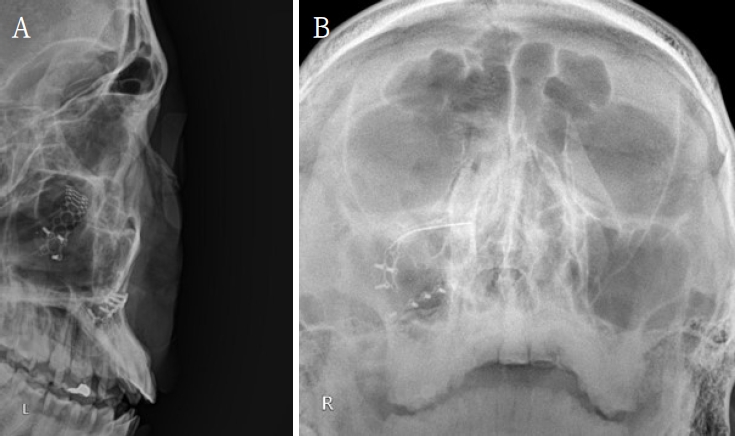
Postoperative radiographs show stable fixation and orbital symmetry. A. Lateral skull radiograph shows intact titanium miniplate fixation of the left orbital floor without displacement. B. Waters’ radiograph demonstrates symmetric orbital outline and stable reconstruction compared with the contralateral side.
Discussion
The management of orbital wall fractures requires a delicate balance between adequate exposure and preservation of orbital function. Among them, orbital floor and medial wall fractures are particularly challenging because of their thin bone structures and proximity to critical orbital contents. Conventional approaches such as subciliary, transconjunctival, or transcaruncular incisions provide access to the fracture site but may cause postoperative complications including visible scarring, eyelid malposition, and infraorbital nerve hypoesthesia [2,4].
In the present case, both the medial and inferior orbital walls were fractured, accompanied by a nasal bone fracture. Considering the extent and location of the fractures, a dual approach was adopted, combining an endoscopic transnasal method for the medial wall and an intraoral transantral approach for the orbital floor. The endoscopic approach allowed excellent visualization of the medial wall through the ethmoid sinus and precise reduction of herniated orbital contents without external incisions. However, due to the inferior wall defect’s position and the need for rigid fixation, the intraoral transantral approach was added. Creating a window on the anterior maxillary wall provided direct access to the orbital floor, enabling accurate reduction and fixation with titanium miniplates and screws.
This combined approach offered several advantages in our patient. It provided sufficient exposure of both fracture sites without external scars or extensive dissection, ensuring stable anatomical restoration and complete resolution of diplopia and ocular discomfort. Postoperative CT confirmed symmetrical orbital contours and stable implant positioning, with no enophthalmos, diplopia, or implant displacement. Only transient infraorbital hypoesthesia was observed, which recovered spontaneously.
Intraoperatively, meticulous hemostasis and careful handling of orbital tissues are essential to prevent bleeding or injury to the infraorbital and ethmoidal neurovascular bundles. Maintaining sinus sterility and ensuring adequate drainage minimize postoperative infection and sinusitis, thereby promoting stable bone healing. Furthermore, attention should be given to potential long-term complications, such as chronic sinusitis, delayed bleeding, or implant displacement. Preventive strategies include gentle manipulation under direct visualization, secure rigid fixation, and proper postoperative follow-up to monitor for late sequelae or bony segment migration.
This case demonstrates that simultaneous use of endoscopic and intraoral approaches can be a safe and effective strategy for complex orbital fractures involving multiple walls. Compared with wide external exposure, this multidisciplinary, minimally invasive method minimizes surgical trauma while ensuring precise reduction and fixation. Particularly in young patients, this approach offers excellent functional recovery and cosmetic outcomes.
The intraoral transantral approach provides direct access to the orbital floor, enabling accurate reduction and rigid fixation while avoiding external scars and minimizing complications. When combined with endoscopic transnasal repair of the medial orbital wall, it offers a conservative and effective strategy for complex orbital fractures. This case demonstrated favorable functional and cosmetic outcomes with minimal complications, supporting the use of these approaches as reliable and safe options in selected patients.
Notes
Conflicts of Interest
None
