Nicolau syndrome following extrusion of endodontic calcium hydroxide: A case report
Article information
Abstract
Calcium hydroxide is commonly used as a root canal disinfectant due to its high alkalinity and biocompatibility. However, excessive injection pressure may cause extrusion beyond the root apex, leading to complications such as nerve or vascular injury. This report showed a case of a 58-year-old woman who developed cutaneous necro-sis and sensory disturbance in the left midface and nasal alar region following endodontic treatment on the left maxillary second molar. Computed tomographic imaging revealed calcified occlusion of the posterior superior alveolar artery. The patient was treated with debridement, stromal vascular fraction injection, and split-thickness skin graft. This case demonstrates a rare but serious complication, known as Nicolau syndrome, resulting from intra-arterial injection of calcium hydroxide. Clinicians should be aware of this potential risk and exercise cau-tion during delivery of intracanal medicaments, especially in vascular-rich anatomical regions.
Introduction
Calcium hydroxide has been generally accepted as an intra-canal medicament during endodontic treatment due to its high alkalinity and biocompatibility [1]. These days, calcium hydroxide pastes are prepared in injection syringe so it can be easily applied in the root canal [2]. However, when calcium hydroxide pastes are injected inside the root canal with high pressure, it can extrude beyond the root apex and cause severe iatrogenic damage [3].
There are several case reports about extrusion of calcium hydroxide paste causing paresthesia of inferior alveolar nerve [3,4], but very few cases describe adverse effects of intra-arterial injection of calcium hydroxide pastes. Unintentional displacement of calcium hydroxide in blood vessels may cause immediate severe pain and the overlying skin rapidly becomes erythematous, violaceous, or blanched. This cutaneous reaction, also known as Nicolau syndrome, can cause necrosis of the skin and underlying tissues to varying extents [5].
Nicolau syndrome is an uncommon adverse reaction that arises at the site of intramuscular drug administration. Initially described in the 1920s in a patient treated with bismuth salts for syphilis, it has since been associated with the intramuscular injection of various agents, including non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and antibiotics [4]. Histopathologic examination typically reveals thrombosis of vessels within the reticular dermis [6].
Although Nicolau syndrome most commonly occurs following intramuscular injections, the present case is unique in that it developed after the extrusion of an endodontic medicament during dental treatment. This report presents a 58-year-old female patient who experienced tissue necrosis and paresthesia of the left nasal and midfacial areas subsequent to endodontic therapy on the left maxillary second molar.
Case Report
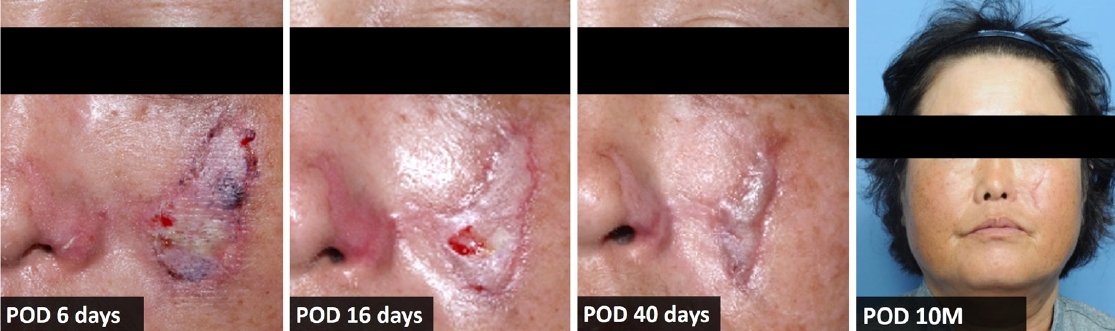
Retrospective data collection, with all patient identifiers removed, was approved by the Institutional Review Board of Kyung Hee University Dental Hospital (IRB No. KH-DT25020). A 58-year-old female patient visited the Emergency Department of Kyunghee University Medical Center with complaints of paresthesia and necrotic change of skin on her left facial area. She has a medical history of diabetes mellitus and latent tuberculosis. She had been undergoing root canal treatment on left maxillary second molar in local dental clinic due to pain. A week ago, canal irrigation and calcium hydroxide paste application on her left maxillary second molar was performed. Immediately after the injection of calcium hydroxide paste, she experienced a tightening facial pain accompanied by bluish discoloration on the skin around her nose. When she presented to the emergency department with necrotic skin changes, a 4.5 cm × 2.5 cm lesion on her left cheek and a 1.5 cm × 1.5 cm lesion on the left nasal alar area were observed during clinical examination (Fig. 1).

Clinical photographs in initial examination show necrotized skin on patient’s left cheek and nasal alar area.
Panoramic view, periapical view and enhanced computed tomography (CT) scan were performed to evaluate the condition further, revealing the extrusion of calcium hydroxide paste over the root apex (Figs. 2A and B). Facial angio CT performed upon presentation to the emergency department showed opacification loss in the branches of the left maxillary artery and skin loss with depression in the left buccal area, without evidence of a fistula tract or subcutaneous inflammation, indicating a possible vascular cause. Based on the findings from the enhanced CT scan, the patient was diagnosed with Nicolau syndrome (Figs. 2C and D).
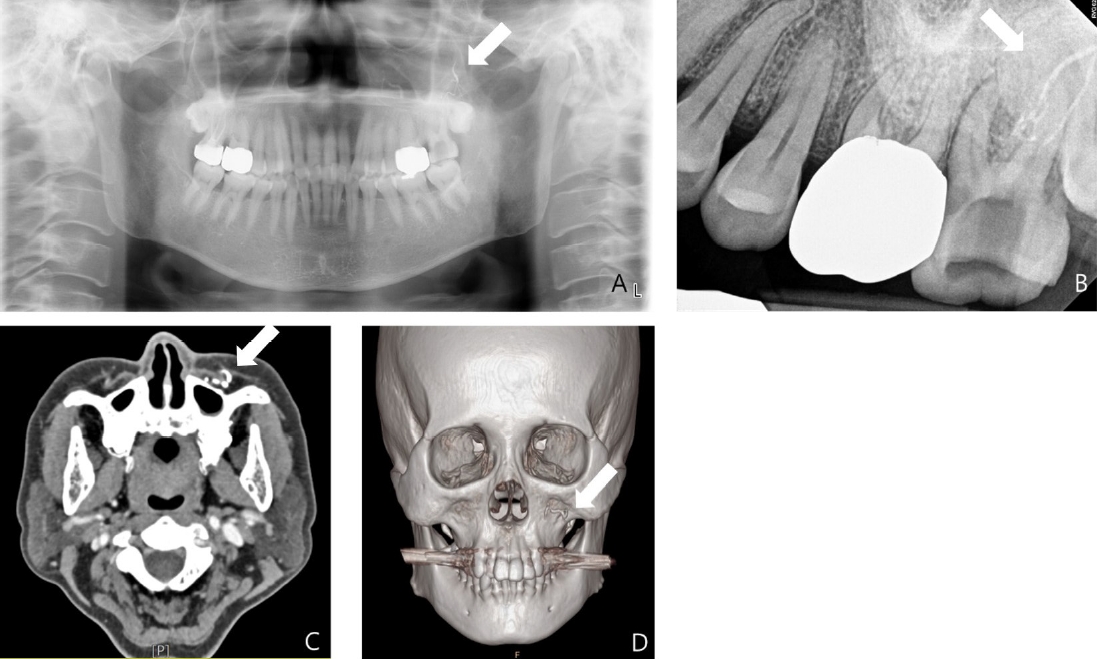
Radiographic examination performed at the initial examination. A and B. Periapical and panoramic views show extrusion of calcium hydroxide paste beyond the root apex of the left maxillary second molar (arrows). C and D. Facial angio computed tomography demonstrate loss of contrast in the posterior superior alveolar artery, indicating arterial obstruction (arrows).
At the emergency department, topical ofloxacin ointment was applied to the necrotic areas and the patient was prescribed medications to alleviate arterial obstruction, including nimodipine 30 mg, aspirin 100 mg, and mecobalamin 0.5 mg. One week after the initial management, debridement and stromal vascular fraction (SVF) injection were performed under local anesthesia and intravenous propofol sedation. For SVF preparation, 100 cc of adipose tissue was harvested from the patient’s left thigh and subjected to centrifugation to isolate the stromal vascular component (Fig. 3).
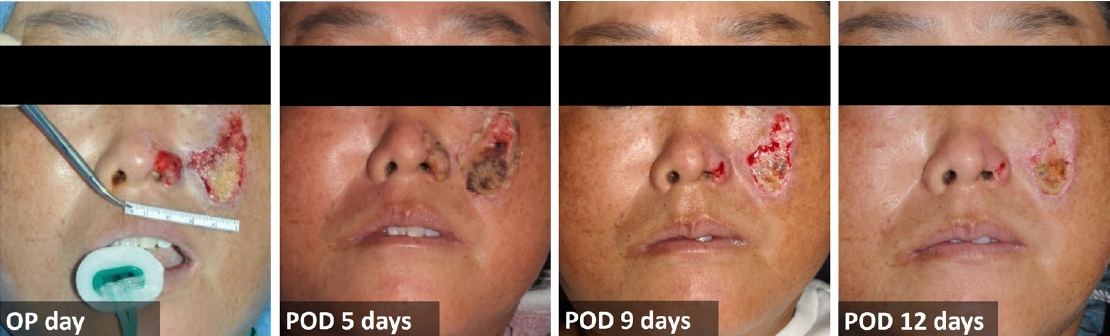
Debridement and stromal vascular fraction injection were performed one week after the initial injury.
After the SVF injection, epithelialization was observed in the nasal area, whereas the midfacial lesion showed clear demarcation with marginal epithelialization. Based on these findings, approximately three weeks after the initial injury, an additional surgical procedure — debridement and coverage with a split-thickness skin graft (STSG) — was performed under local anesthesia. A split-thickness skin graft harvested from the left temporal scalp was used to cover the cheek defect (Fig. 4). Furthermore, the left maxillary second molar was extracted, as it was determined to have a poor prognosis due to severe palatal alveolar bone resorption. Throughout the postoperative follow-up period, the wound demonstrated satisfactory healing without evidence of infection; however, scar formation was noted (Fig. 5). Due to the aesthetic importance of the facial region, a third surgical procedure for scar revision was performed three months after the initial operation.

The patient subsequently underwent a second surgical procedure, consisting of debridement (A), harvest of a split-thickness skin graft from the left temporal scalp (B), and coverage of the wound with the graft (C).
Discussion
In this report, the patient developed extensive skin necrosis and neuropathic symptoms following inadvertent extrusion of calcium hydroxide during endodontic treatment, consistent with Nicolau syndrome. The pathophysiology of this syndrome remains incompletely understood, but several plausible mechanisms have been suggested. First, vasospasm triggered by sympathetic nerve stimulation may lead to tissue ischemia. Second, accidental intra-arterial injection of drugs can result in thromboembolic obstruction. Third, perivascular or intravascular injection may cause inflammation and progressive intimal damage, leading to arterial wall necrosis and soft tissue infarction. Despite their differences, these mechanisms converge on a final common pathway: ischemia [5]. Histopathologic findings in reported cases support these theories, demonstrating widespread fibrin thrombi within dermal vessels, ischemic necrosis of eccrine glands, and fat necrosis adjacent to thrombosed vessels, consistent with vascular occlusion as the primary insult [6].
The potential for Nicolau syndrome may exist with any injectable agent, especially when administered under high pressure or in anatomically vascular regions. Although Nicolau syndrome is most commonly reported after intramuscular drug injections, few cases have been described in dental literature, nearly all related to calcium hydroxide extrusion. Calcium hydroxide has been widely used in endodontics since its introduction by Hermann in 1920, owing to its high pH (~12.5), antimicrobial effects, and ability to induce hard tissue formation [1,2]. However, its high alkalinity may induce chemical vasospasm or direct cytotoxic damage to endothelial cells, leading to local thrombosis [4]. In this case, facial angio CT revealed abrupt loss of contrast in branches of the left maxillary artery, supporting a vascular etiology.
There is currently no universally established treatment protocol for Nicolau syndrome, and therapeutic approaches are largely based on clinical experience. Common strategies include the use of analgesics to control pain, corticosteroids to suppress inflammation, and antibiotics to prevent secondary infections. In some reports, thrombolytic and anticoagulant therapies have been initiated early in an attempt to reduce the extent and severity of ischemic necrosis [4,7]. Pharmacologic management in this case included the use of nimodipine (calcium channel blocker) and aspirin to improve microcirculation and prevent further thrombotic progression [4,5]. Antibiotics were prescribed to prevent superimposed infection in necrotic tissue, and mecobalamin was administered to alleviate neuropathic symptoms. Despite the initial treatment, the severity of the tissue damage required several surgical procedures, including debridement, injection of SVF, and STSG. In this case, SVF therapy was undertaken as a compassionate, clinically necessary intervention with written informed consent from the patient. Autologous SVF was harvested from subcutaneous adipose tissue in the patient’s left thigh and injected into the necrotic region to facilitate wound healing. SVF is a regenerative cell product derived from adipose tissue and obtained through enzymatic digestion and centrifugation. It comprises a heterogeneous mixture of adipose-derived stem cells, endothelial progenitor cells, pericytes, fibroblasts, and immune cells [8]. Acting primarily through paracrine signaling, SVF secretes growth factors, cytokines, and extracellular vesicles that modulate inflammation, promote angiogenesis, and support tissue regeneration [8].
Continued radiographic detection of extruded material even weeks after trauma further underscores the importance of prevention over management (Fig 6.). This case emphasizes the need for careful technique and an awareness of anatomic risk zones during endodontic procedures. Although most reported cases of Nicolau syndrome in dentistry have involved maxillary molars due to their proximity to major arteries, a recent report by Kang et al. [7] (2024) demonstrates that Nicolau syndrome can also occur following root canal treatment of mandibular molars. This highlights the fact that clinicians must maintain vigilance regardless of the tooth involved.
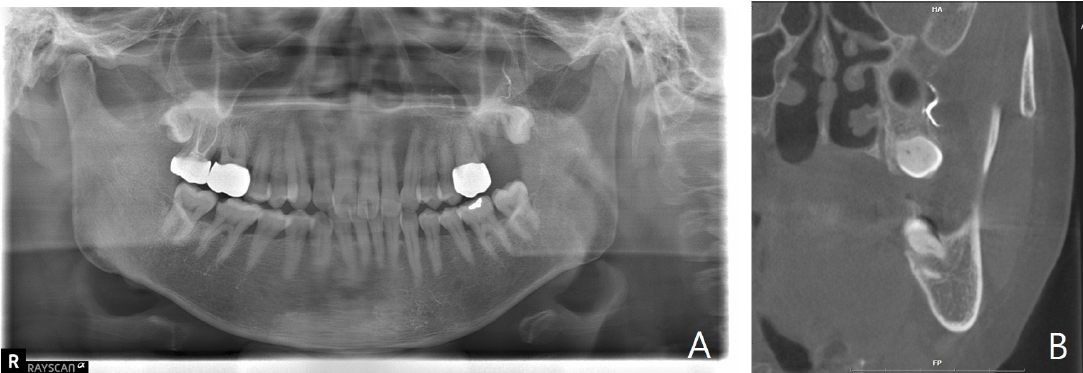
A. Panoramic radiograph taken approximately six weeks after the incident shows persistent radiopaque material in the periapical region, consistent with extruded calcium hydroxide. B. Coronal cone-beam computed tomogrpahic image demonstrates the presence of extruded calcium hydroxide within the adjacent soft tissue space.
To minimize the risk of Nicolau syndrome during endodontic procedures, several preventive measures are recommended. First, low-pressure techniques should be employed for intracanal medicament delivery, preferably using a lentulo spiral or hand files rather than syringe injection. Second, the working length should be precisely confirmed using apex locators and periapical radiographs. Third, in high-risk teeth (e.g., maxillary molars), preoperative CBCT imaging may be considered to evaluate the proximity to arterial structures. Finally, injection should be stopped immediately if resistance is encountered or the patient reports sudden severe pain.
This case highlighted a rare but severe complication of endodontic treatment — Nicolau syndrome — leading to vascular occlusion of the posterior superior alveolar artery and extensive midfacial necrosis. Early recognition and prompt multimodal management, including pharmacologic therapy to improve microcirculation, autologous SVF injection to stimulate wound healing, and reconstructive surgery with split-thickness skin grafting, are critical to minimize favorable functional and aesthetic outcomes.
Notes
Conflicts of Interest
None