Iatrogenic extrusion of endodontic materials into the inferior alveolar nerve during endodontic procedures: A case series
Article information
Abstract
This case series analyzes five patients treated at the Department of Oral and Maxillofacial Surgery at Kyung Hee University Dental Hospital for iatrogenic inferior alveolar nerve injuries caused by the extrusion of endodontic materials (calcium hydroxide paste and an MTA-based sealer). The study evaluates the clinical characteristics, symptom onset, anatomical injury distribution, and treatment outcomes for each case. By identifying patterns in radiographic and symptomatic findings, it aims to clarify the degree of nerve involvement and explores how the physicochemical properties of each material affect the perineural space. Through a review of recovery patterns following both surgical and conservative management, the report serves as a practical reference for clinicians. Ultimately, it emphasizes the critical importance of meticulous technique in root canal procedures and the ne-cessity of timely diagnostic imaging when nerve injury is suspected.
Introduction
Endodontic treatment is a common dental procedure performed to treat diseases of the dental pulp and surrounding periapical tissues. A fundamental aspect of this treatment involves the use of intracanal medications and sealers. Calcium hydroxide paste (e.g., Calcipex II) and mineral trioxide aggregate (MTA)-based sealers are widely utilized for their antibacterial properties, sealing capacity, and biocompatibility [1]. Calcipex II (J Morita, Osaka, Japan), a water-based paste, is valued for its ease of delivery and effectiveness in microbial reduction. EndoSeal MTA (Maruchi, Wonju, Korea), a premixed injectable sealer, is known for its sealing properties and minimal tissue toxicity.
These materials are designed to remain confined within the root canal system. However, complications may arise when they are inadvertently extruded beyond the apical foramen, especially in cases involving over-instrumentation, perforation, or excessive pressure during insertion. When such materials enter the mandibular marrow space or directly contact the inferior alveolar nerve, they may cause inflammatory responses, chemical irritation, and mechanical compression 2) . These factors can result in varying degrees of neurosensory dysfunction, including paresthesia or anesthesia.
This report described 5 patients who sustained iatrogenic injuries to the inferior alveolar nerve (IAN) due to extrusion of endodontic materials. Four patients were affected by Calcipex II, while one case involved EndoSeal MTA. Clinical and radiographic findings, treatment approaches, and postoperative outcomes are reviewed, and potential mechanisms of nerve injury are discussed.
Case Report
This study was approved by the Institutional Review Board (IRB) of Kyung Hee University Dental Hospital. (KH-DT25021)
Case 1
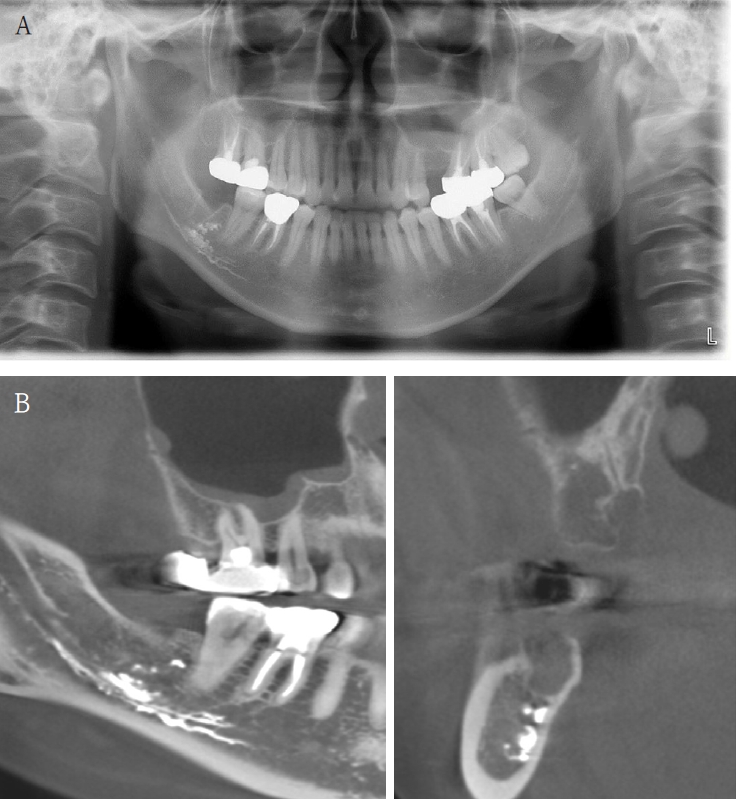
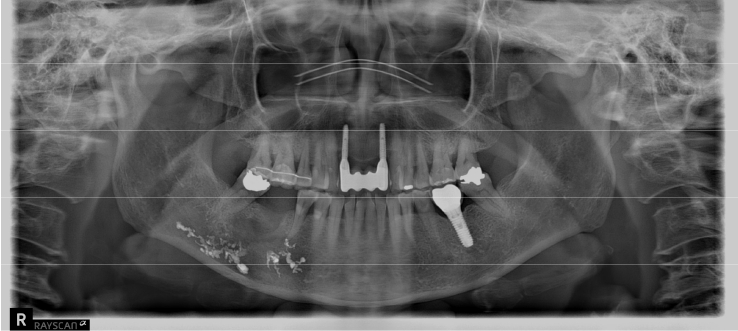
A 63-year-old female presented three days after endodontic treatment of the mandibular left second molar (#37) with symptoms of numbness in the left lower lip and gingiva. A panoramic radiograph and cone-beam computed tomography (CBCT) revealed extrusion of Calcipex II into the mandibular canal (Fig. 1). Initial neurosensory testing demonstrated mild hypoesthesia. She was admitted for foreign body removal and neurorrhaphy under general anesthesia. A post-operative panoramic radiograph confirmed the removal of the foreign body (Fig. 2). Although surgical curettage and neurorrhaphy were performed on the fourth day post-onset, no significant symptom relief was noted at the one- and two-week follow-ups. At the three-month follow-up, she reported persistent numbness with mild neuropathic discomfort but no marked improvement. A follow-up neurosensory exam is scheduled for the six-month check-up.
Case 2
A 41-year-old female reported persistent numbness in the right lower lip and chin following endodontic treatment of the mandibular right second molar (#47). A panoramic radiograph and CBCT revealed extrusion of Calcipex II into the IAN (Fig. 3). She declined surgical intervention and was treated conservatively with mecobalamin and gabapentin. Serial follow-ups at one and three months showed no clinical improvement.
Case 3
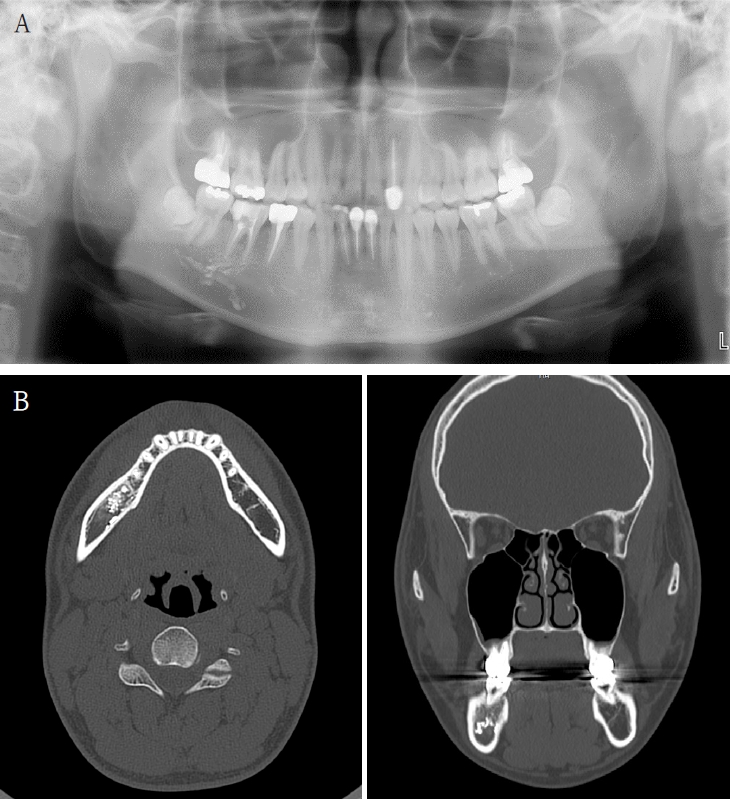
A 61-year-old female presented with intermittent right mandibular swelling and pain after root canal therapy was done using EndoSeal MTA 5 months ago. A panoramic radiograph, CBCT and bone scan confirmed material extrusion and mild localized bone changes (Fig. 4). Initial neurologic evaluation demonstrated nearly normal sensory function, with Visual Analog Scale (VAS) 4 discomfort. Surgical curettage was performed under local anesthesia. A post-operative panoramic radiograph confirmed the substantial removal of the foreign body (Fig. 5). Postoperatively, the patient reported significant improvement at both the one- and two-month follow-ups. Due to full symptom resolution, no follow-up neurosensory testing was performed.
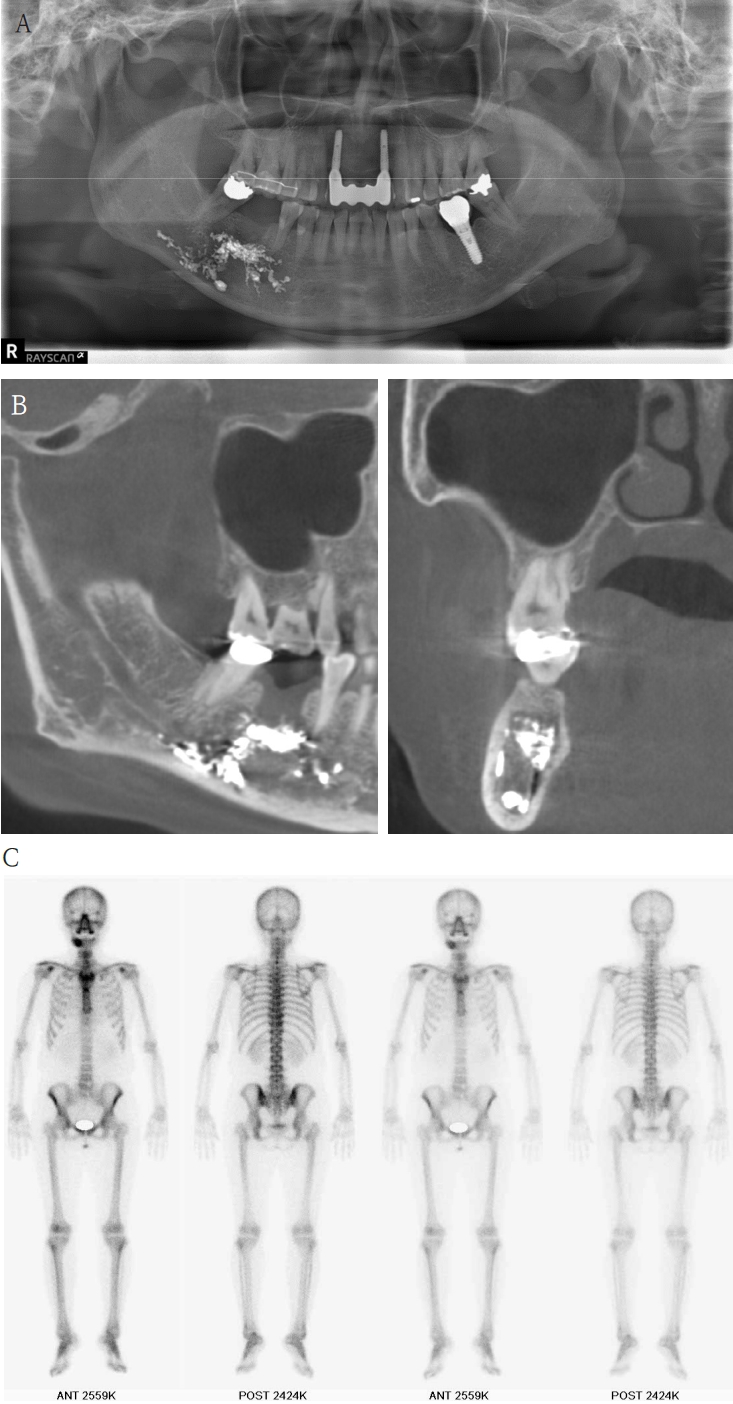
A. Pre-op panoramic radiograph of Case 3 patient. B. Pre-op CBCT of Case 3 patient. C. Pre-op bone scan of Case 3 patient
Case 4
An 18-year-old male developed numbness in the right lower lip, gingiva, and chin following endodontic treatment of the mandibular right first molar (#46) at a military hospital 2 weeks ago. A panoramic radiograph and multi-detector computed tomography (MDCT) revealed extruded Calcipex II in proximity to the IAN (Fig. 6). Neurologic testing confirmed severe hypoesthesia in the right mentum region. Thermal discrimination was absent across a broad area of the right lower lip and chin. The patient’s subjective discomfort was rated as VAS 2. The patient underwent foreign body removal, nerve transposition, and bone grafting under general anesthesia (Fig. 7). At one-week postoperative follow-up, neurosensory testing showed little to no improvement. At the five-month follow-up, repeated neurosensory testing demonstrated meaningful improvement in directional discrimination and pin-pressure nociceptive discrimination, despite the continued presence of hypoesthesia. At the 17-month follow-up, testing revealed further improvement, including recovery of static light touch sensation, with overall symptoms classified as mild hypoesthesia. However, the patient reported worsening subjective discomfort, with a VAS 5, reflecting a discordance between objective sensory recovery and subjective symptom persistence.
Case 5
A 73-year-old male was referred after endodontic treatment of the mandibular right second molar (#47) with severe post-treatment pain. Evidence of Calcipex II extrusion into the IAN canal was evident on the panoramic radiograph and CBCT. (Fig. 8). Root canal treatment was done about 2 months ago. He underwent foreign body removal under general anesthesia (Fig. 9). Postoperatively, he reported minimal change in numbness symptoms. He was lost to follow-up but returned six months later complaining of recurrent neuropathic symptoms and itching. Carbamazepine was prescribed. No follow-up sensory testing was performed.
Discussion
The inferior alveolar nerve is anatomically vulnerable during endodontic procedures, particularly in the posterior mandible where tooth roots are close to the inferior alveolar canal 3) . When endodontic materials are extruded beyond the root apex, direct contact with the IAN can result in damage through several mechanisms, largely influenced by the chemical and physical properties of the material involved.
Calcipex II, primarily composed of calcium hydroxide, has a highly alkaline pH of approximately 12.5 [4]. This high pH creates a hostile environment for neural tissue, contributing to demyelination and axonal injury. Histologically, this can appear as axonotmesis, characterized by disruption of axons with preservation of the endoneurial sheath, leading to sensory disturbances. Additionally, alkaline-induced protein denaturation, lipid peroxidation, and local ischemia may amplify nerve injury [5]. Reports suggest that hydroxyl ions released from calcium hydroxide can penetrate perineural structures, causing edema and direct neurotoxicity [6].
In contrast, EndoSeal MTA has a pH ranging from 10 to 11 and is generally considered more biocompatible. However, its extrusion in excessive quantities, particularly in premixed or over-pressurized forms, may lead to adverse tissue responses. Although MTA exhibits lower cytotoxicity, its physical presence in confined spaces such as the mandibular canal can elicit a foreign body reaction, chronic inflammation, and mechanical compression of the nerve. Studies have documented perineural fibrosis and delayed healing in response to bulk MTA accumulation, indicating that even biocompatible materials can cause significant pathology under inappropriate conditions [7].
The clinical presentation of profound hypoesthesia or anesthesia, as observed in Cases 1, 2, 4, and 5, is consistent with axonotmesis [8] (a Sunderland second-degree injury 9) ). The chemical neurotoxicity from calcium hydroxide likely caused severe disruption of the axons themselves, while leaving the surrounding connective tissue sheaths (endoneurium) largely intact. This disruption interrupts the afferent signal transmission from the sensory receptors in the lip and chin to the central nervous system, resulting in the clinical finding of numbness. While the preserved endoneurium provides a scaffold for potential regeneration, the initial chemical insult is severe enough to cause a complete loss of function in the affected axons.
Furthermore, the neuropathic symptoms reported, such as the mild discomfort in Case 1 and the worsening VAS score despite objective sensory recovery in Case 4, point towards a more complex pathophysiology beyond simple nerve conduction block. This phenomenon can be attributed to aberrant nerve regeneration and central sensitization. Following axonotmesis, regenerating nerve fibers can sprout abnormally, forming disorganized connections or small neuromas that lead to spontaneous, ectopic firing [10]. This disorganized healing process generates faulty signals that the brain interprets as pain, tingling, or discomfort [11]. The paradoxical outcome in Case 4 perfectly illustrates this disconnect, where objective sensory function improves as some axons successfully reinnervate their targets, while subjective pain worsens due to the pathologic activity of other improperly regenerating fibers.
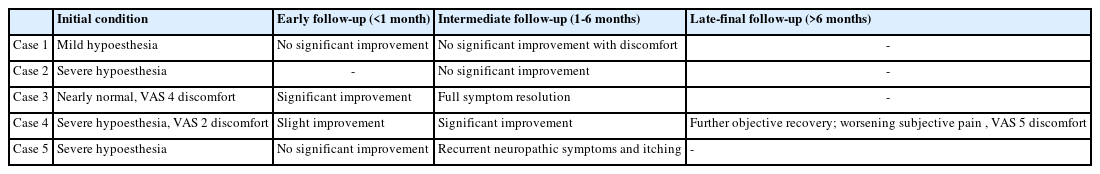
As demonstrated in Tables 1 and 2, the clinical outcomes in this case series provide several insights into the management of IAN injuries from endodontic material extrusion. Notably, conservative management was unsuccessful in the one patient who declined surgery (Case 2) and showed no clinical resolution. In contrast, surgical intervention yielded variable results that were not strictly dependent on timing. For example, Case 3 demonstrated that a successful outcome is possible even when surgery is delayed by as much as 5 months. This stands in contrast to Case 1, where early intervention at 7 days did not lead to resolution, suggesting the initial severity of the injury may be a more critical prognostic factor than the timing of intervention alone. Finally, the recovery process itself can be multifaceted, as highlighted by the unique outcome in Case 4 (Resolution: Δ). This case illustrates a significant discordance between objective sensory recovery and subjective symptomatic experience, a crucial consideration for clinical practice.
From a clinical perspective, unintentional extrusion of endodontic materials into the inferior alveolar nerve represents a serious clinical complication with the potential to cause long-lasting or irreversible neurosensory deficits. The variability in recovery trajectories emphasizes the need for early detection and individualized treatment planning. Conservative management may suffice in select cases without direct nerve involvement, but persistent symptoms or radiographic evidence of nerve contact should prompt consideration of surgical intervention.
Clinicians should exercise heightened caution when using intracanal medicaments and sealers in mandibular molars that are anatomically close to the IAN. Immediate CBCT imaging is advisable when patients present with neurosensory symptoms following endodontic procedures, as it aids in the identification and localization of extruded materials.
This case series highlights the importance of careful procedural technique, early diagnosis, and appropriate intervention, especially in posterior mandibular teeth where proximity to the neurovascular bundle increases the risk of iatrogenic injury. Clinicians should maintain careful clinical oversight and refer promptly for surgical evaluation when nerve injury is suspected.
Notes
Conflicts of Interest
None