Clinical trial of platelet rich fibrin insertion for exposed dental pulp of second molar associated with impacted third molar: A pilot study
Article information
Abstract
Purpose
Root resorption of second molars (M2s) due to impacted third molars (M3s) can result in pulp exposure of second molars. Platelet rich fibrin (PRF) has recently been investigated because of its positive effect on tissue healing. This study aims to determine the clinical utility of applying PRF to pulp exposure site of second molars affected by impacted third molars using radiological and clinical examination.
Materials and Methods
Ten patients with exposed pulp of M2 by impacted M3 were evaluated clinically and radiographically before surgery. Extraction of M3 was performed and average follow up period was 8.3 months (ranged from 1 week to 40 months). Extraction was done using conventional method and PRF was applied to pulp exposure site. PRF was obtained by collecting the patient’s blood and spinning it in a centrifuge at 1300 RPM for 15 minutes. After extraction of M3, clinical and radiographic exam was done regularly to evaluate dentin bridge formation, bony healing and viability of M2.
Results
In 6 of 10 patients who underwent regular follow-up, dentin bridge formation and bony healing were ob-served radiographically at the site of PRF application. All patients remained free of symptoms implying additional external root resorption or pulp necrosis.
Conclusion
This study shows that the application of PRF on M2 pulp exposure site associated with impacted M3 is effective in promoting healing. Although this study demonstrates beneficial effect of PRF, further controlled studies are warranted.
Introduction
Pressure associated with impacted third molars (M3) occasionally result in external root resorption (ERR) of adjacent second molars (M2) [1-3]. The main etiologies of ERR is known as periodontal ligament injury [4,5]. ERR associated with mandibular M3 is reported with various incidence which ranges from 20.17 to 52.9% [6-8]. And ERR associated with maxillary M3 is reported less frequent than in mandible [6,9]. Additionally, male, old age, depth and angle of impaction are known as risk factors for ERR [2,3,6-10]. Regarding the location of ERR, cervical ERR was prevalent in mandibular M2 and apical ERR was prominent in maxillary M28].
Regarding severity of ERR, severe ERR involving root canal exposure was prevalent in middle and apical third of a M2 root [10]. Incidence of severe ERR has been reported 16.7% in maxilla and 23.9% in mandible [11]. Symptoms of ERR are known as severe pain, allodynia on temperature, mobility, apical periodontitis, alveolar bone resorption, and root fracture [12,13]. Despite majority of M2 with root canal exposure are asymptomatic, about 10% of patients experienced mentioned discomfort [13].
Even though affected M2 are able to be treated with root canal treatment or extraction, it will be possible to prevent of this problem at the time of extraction. Several materials such as Biodentine™ (Septodont Ltd, Saint Maur des Faussés, France), calcium hydroxide, mineral trioxide aggregate, IRoot™ BP (Innovative BioCeramix Inc, Vancouver, Canada) are reported effective for treatment of exposed pulp [14]. Despite their well-known efficacy, it might be difficult to apply exactly on exposed M2 root canal adjacent to M3 extraction socket and its effect on extraction socket is uncertain.
Several studies have demonstrated that growth factors such as transforming growth factor βs, bone morphogenetic proteins, insulin growth factor, platelet-derived growth factor and vascular endothelial growth factor are significant in dentin-pulp recovery [15-17]. And its clinical efficacy was shown in previous studies [18,19]. Additionally, growth factors can promote healing potency of extraction socket [20]. Platelet-rich fibrin (PRF) is a concentrate of fibrin, platelet and growth factors derived from patient’s blood and is a well-established biomaterial for delivering such growth factors to injured sites. PRF is extensively utilized in dentistry including oral surgery, regenerative endodontic therapy and periodontal therapy [21]. As a result, the application of PRF to the exposed M2 root canal and the adjacent M3 extraction socket is expected to be beneficial. However, scientific evidence supporting the therapeutic role of PRF remains limited.
Therefore, the aim of this study was to prove benefits of PRF in treatment of M2 root canal exposure induced by impacted M3 with the radiographical and clinical investigation.
Materials and Methods
This study was approved by the institutional review board (IRB) of Yonsei university dental hospital (IRB No.2-2025-0302).
Selection of patients
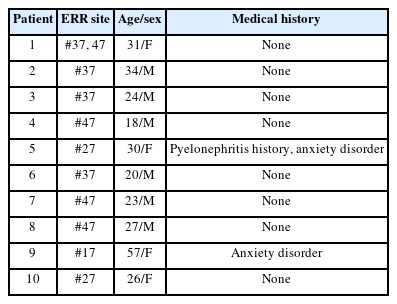
Ten patients who visited outpatient clinic of Department of Oral and Maxillofacial Surgery in Yonsei University Dental Hospital from April 2021 to April 2025 were selected. All included patients visited clinic for impaction or cystic lesion on M3 and ERR of all cases were verified on panoramic radiography or cone-beam computed tomography (CBCT). All patients exhibited ERR involving the dental pulp of M2 due to an adjacent impacted M3. The presence of ERR was determined when definitively destructive radiolucent pattern extended to root canal was observed on M2 root adjacent to M3 on panoramic radiography and CBCT. None of patients had systemic disease affecting ERR (Table1).
Surgical procedure
Surgical extraction of M3 was performed by a single surgeon. After enucleation of any associated cysts and re moval of granulation tissue, the operator clearly identified exposed dental pulp. On pulp exposure site, platelet rich fibrin (PRF) was applied. PRF was obtained by centrifuging 20ml of the patient’s venous blood at 1300 RPM in 15 minutes. PRF covered entire root surface of M2 and floor of M3 extraction socket. Above PRF, Ateloplug® (Hyundai Bioland, Cheongju, Korea) was packed in extraction socket for hemostasis and stable application of PRF. After that, operation site was sutured with single interrupted method. Dentigerous cysts were identified intraoperatively in 4 cases and in such cases, the size of cysts was similar to a crown of M3.
Evaluation of efficacy of PRF
To assess dentin bridge formation and bone healing, clinicians evaluated radiolucent calcification around the ERR site of M2 and increased radiopacity around the extraction area on postoperative panoramic radiographs. Postoperative panoramic radiography was taken at round a week, 4 months and then every 6months thereafter. Average follow up period was 8.3 months ranged from 1 week to 40 months. Clinical signs of pulp necrosis and progression of ERR, including increased tooth mobility, pain, infection, or hypersensitivity, were also eval uated. No additional surgical damage was observed in any case.
Results
In 6 of 10 patients, dentin bridge formation and bone healing at the PRF application site were visible on panoramic radiographs (Figs. 1 and 2), excluding 4 patients who returned only once within one month postoperatively. In Table 2, patients who presented radiographic improvement and patients who had uncertain radiographic results due to insufficient follow-up period were described. In addition to bony healing, dental pulp atrophy was detected in a case (Fig. 3). No additional ERR was observed in any patients. Only one patient had preoperative and postoperative CBCT, and dentin formation and bony healing was seen on CBCT 6 months after surgery.

Bony healing and dentin bridge formation is visible on post operative panoramic radiographies (B, D, and F) compared to preoperative panoramic radiographies (A, C, and E). A. Pre-operative panoramic radiograph of left lower third molar. B. Panoramic radiograph of left lower third molar after 11 months of surgery. C. Pre-operative panoramic radiograph of right lower third molar. D. Panoramic radiograph of right lower third molar after 14 months of surgery. E. Pre-operative panoramic radiograph of right upper third molar. F. Panoramic radiograph of right lower third molar after 11 months of surgery.
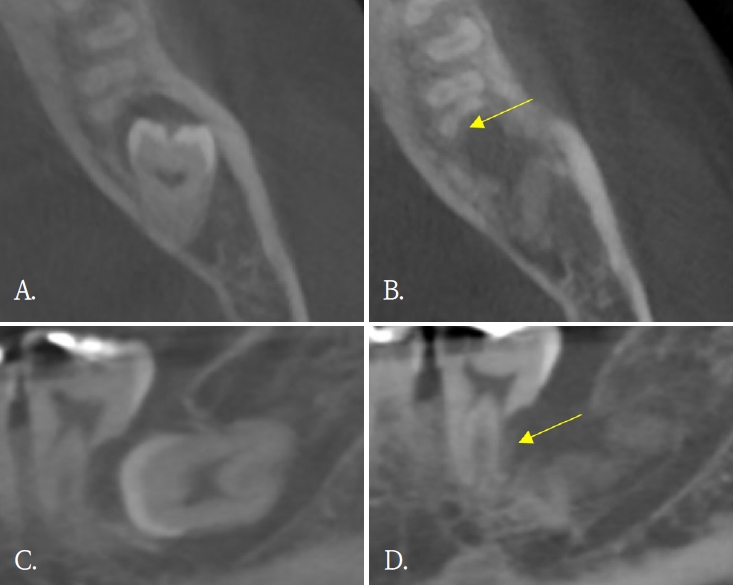
Dentin formation (yellow arrows). A and C. Pre-operative cone-beam computed tomographic (CBCT) images. B and D. Post-operative CBCT after 6 months of surgery.
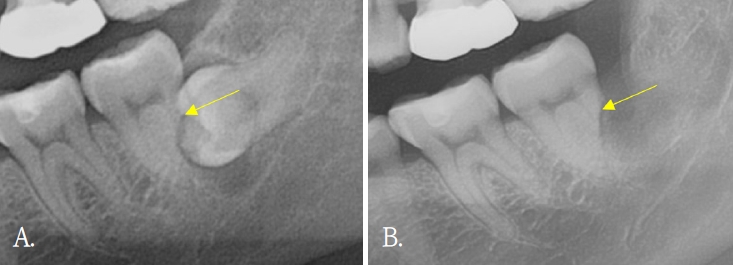
Pulpal atrophy with apex closure is visible on postoperative panoramic radiography (yellow arrows). A. Pre-operative panoramic radiography. B. Panoramic radiography after 4 months of surgery.
None of the patients reported symptoms such as in creased mobility, pain and hypersensitivity on first follow up visit. And all patients did not undergo extraction or endodontic treatment on affected M2. One patient developed a postoperative infection, which was success fully managed with cephalosporin and ibuprofen medication for a week (Table 2).
Discussion
Since its introduction in dentistry by Choukroun et al., PRF has been widely investigated in various fields such as oral and maxillofacial surgery, periodontology and im plantology [22-24]. Because of its cost-effectiveness, ease to preparation and excellent biocompatibility, PRF is suit able for a wide range of clinical application [25]. This pilot study explores clinical possibility of PRF on ERR site of M2 associated with impacted M3 and it makes clear distinction from previous studies which reported application of PRF on bone regeneration of extraction socket or pulp capping [19,20]. Despite the difference in application site, this study also demonstrated positive clinical results. The results of this study can serve as reliable evidence for more active utilization of PRF on ERR site of M2 associated with M3 and for conducting further related research.
The results of this study imply positive effect of PRF on ERR site of M2 associated with impacted M3. However, to verify clinical efficacy of PRF more accurately, this study needs further refinement. First, the period of radiographical evaluation needs to be standardized. In this study, the follow-up periods for radiographic evaluation varied among patients, and 4 patients lacked adequate follow up to detect meaningful changes. Further studies should include patients with long-term, standardized follow-up. Second, the modality of radiographic exam needs to be improved. CBCT is known to provide higher resolution and accuracy than panoramic radiography [26,27]. But not all the patients underwent postoperative CBCT. Eventually, the clinician determined favorable healing only with panoramic radiography and symptoms. To more precisely evaluate radiographic change, further studies need to contain preoperative and regular postoperative CBCT. Third, a control group or comparative study design is needed to accurately evaluate the effect of PRF. Comparable materials for further studies may include collagen plug, growth factors, newly introduced scaffolds or stem cells derived from various part of body. Lastly, method to evaluate the viability of M2s needs to be quantified. In this study, only qualitative evaluation was used to evaluate viability of M2s. Methods including the electric pulp test (EPT), regular quantitative recording of mobility and hypersensitivity are required in further studies.
Although most M2s with ERR heal asymptomatically, complications such as pain, residual root fracture, allodynia may occur in some of M2. Furthermore, Qu et al. [13] demonstrated that older age increases the risk of such complications. According to the “Dental Outpatient Visit Trends” report published by the Health Insurance Review and Assessment Service (HIRA) in 2023, the age of patients visiting dental clinics is showing an increasing trend, possibility of harmful symptoms on ERR site associated with M3 also may increase. The efforts to improve healing of ERR site of M2 associated with impacted M3 will prevent requirement for unnecessary root canal treatment or extraction. The results of this pilot study and further studies based on this study may provide a reliable solution.
In conclusion, 6 patients who had sufficient follow up duration showed radiographic improvements, such as dentin bridge formation and bony healing, were observed in all 6 patients within follow-up period. No patients demonstrated clinical symptoms requiring further intervention. These findings suggest that PRF may enhance the healing potency of ERR site of M2 associated with impacted M3.