Implications of Japan's 8020 Campaign and the Current Status of Oral Health in the Elderly of Korea and Japan
Article information
Abstract
As the first nation to experience a super-aging society, Japan’s response measures have various implications. To improve the oral health of the elderly, the Japanese central government, local governments, and the dental community collaborated in 1989 to launch the 8020 Campaign, aiming for individuals to maintain 20 teeth at 80.
This campaign has yielded significant improvements in the oral health of the elderly. Initially, at the beginning of the 8020 campaign, only 7% of those aged 80 had 20 or more teeth, with an average of 4–5 teeth. By 2011, 22 years after its inception, the achievement rate increased significantly to 38.3% and reached 51.6% in 2016, exceeding the initial target of 50%. The fact that the 8020 campaign achievers improved their oral health and improved various systemic health indicators, including reductions in total mortality and noninfectious diseases, has been supported by various research findings. As a first step in applying Japan’s 8020 Campaign experience to Korea, we compared the rate of possessing 20 or more present teeth and the average number of present teeth among elderly individuals aged 75–79. In 2000, 30.4% of the Korean elderly individuals had 13.1 teeth on average, while for the Japanese elderly individuals (1999 data), it was 17.5% with an average of 9.0. However, this trend was reversed by 2011, with elderly Japanese surpassing Koreans in rate of retaining 20 or more teeth average number of teeth present. The most recent survey in 2022 showed that Japanese elderly individuals lead with a 55.8% rate of retaining 20 or more teeth and an average of 18.1 teeth, compared with Korean elderly individuals (2019 data) at 53.9% possession and 17.3 teeth on average, respectively.
Based on Japan’s successful experience, Korea must collaborate with the central government and dental community to establish ambitious and concrete oral health goals and to sustain efforts to achieve them. This study provides policy insights into promoting oral health among older adults by analyzing and comparing the oral health status of older adults in Korea and Japan through Japan’s 8020 campaign.
Ⅰ. Rapid Aging in Japan and Korea
Japan has the fastest aging population in the world, with 29.1% of its population aged 65 years or older as of 2022. This percentage is expected to increase to 34.8% by 2040 [1]. Korea is now significantly surpassing Japan’s aging rate. Between 2010 and 2020, Korea’s growth rate in the elderly population was 4.2%, more than double that of Japan (2.1%). Korea became an aging society in 2000, with over 7% of its population aged 65 years or older. By 2018, this increased to over 14% of the population. South Korea is projected to become a super-aged society by 2025, with over 20% of its population aged 65 years or older. South Korea’s aging rate is expected to reach 30% by 2035 and 37% by 2045, making it the world’s leading aging country, surpassing Japan [2].
It is also possible to compare the aging rates in Japan and South Korea using the aging index, which is another indicator of the rate of increase in the elderly population. As of 2020, Japan’s aging index was 248.3, and South Korea’s was 129.3, which is half that of Japan. However, South Korea’s aging rate is progressing much faster than that of Japan. By 2030, Japan’s aging index will reach 293.8, but South Korea will surpass Japan at 301.6 [3].
Furthermore, Korea has one of the lowest fertility rates globally and is expected to accelerate its transition to an aging society. Therefore, the existing definition of the elderly needs to be revised or redefined from a uniform standard of 65 years or older, and there is an urgent need for social attention and policy support for healthy aging, ensuring that the elderly are in good health without suffering from diseases.
Ⅱ. Necessity for Segmentation of the Elderly Population
Classifying human life into specific age groups according to the life cycle is more effective for developing and applying customized policies appropriate for the target age group. For example, we have specific age segments: infants (1 month to 1 year), toddlers (1~7 years old), children (8~17 years old), young adults (19~34 years old), middle-aged (35~49 years old), and seniors (50~64 years old). However, the elderly, who constitute a large portion of the population, are grouped together as seniors.
Globally, the definition of the elderly as 65 years of age or older is said to have originated in the 1950s, when the United Nations used it as the basis for calculating age indicators [4]. In Korea, the perception of the elderly as 65 years of age or older was generalized when the Elderly Welfare Act of 1981 applied preferential treatment to those aged 65 and older.
However, the need to categorize the elderly into specific age groups has been advocated by those studying geriatrics. Louise Aronson, a leading researcher in gerontology, proposed that instead of lumping people over 65 together as the elderly, they should be categorized into the following age groups: those in their 60s as younger elderly, those in their 70s as older elderly, those in their 80s as frail elderly, and those in their 90s and above as very old elderly. Furthermore, to consider the level of independence and dependence of the elderly, those in their 60s and 70s were categorized as independent, while those over 80 were categorized as dependent elderly [5].
As life expectancy in Korea has significantly increased over the past few decades, older adults have begun to recognize the need to redefine their age. According to the 2020 Senior Citizen Survey conducted by the Ministry of Health and Welfare in Korea, 52.7% of Korean seniors consider 70~74 years to be the age at which old age begins [6].
Therefore, instead of the current one-size-fits-all approach of defining the elderly as those over 65 years old, we must raise the threshold for the elderly, subdivide them into age groups, and establish specific health goals for each group.
Ⅲ. Necessity for Health-oriented Oral Function Evaluation Indicators
An increase in the elderly population is inevitably accompanied by an increase in healthcare costs. For dental caries and periodontal disease, representative oral diseases, the caries experience index of permanent teeth (DMFT) and community periodontal index (CPI) have been used as epidemiological evaluation indices. The DMFT index, introduced by Klein and Palmer in 1940 [7], comprehensively measures dental caries experience by integrating decayed, filled, and teeth lost due to caries. The DMFT for 12-year-old children, marking the completion of permanent dentition, is globally used as a standard statistic to compare oral health across countries. Based on this, the World Health Organization (WHO) proposed a specific goal in 2000 to reduce the DMFT of individuals aged 12 years to < 3.0. The Community CPI, established in 1982, was designed to compare the status of periodontal diseases across countries. Initially, the treatment needs component Community Periodontal Index & Treatment Need (CPITN), which has recently been used as a CPI alone, excluding treatment needs [8]. However, both the DMFT and CPI indices assess dental caries and periodontal disease status rather than reflecting a healthy oral state or function. A representative limitation of the DMFT index is that the weights of decayed, filled, and missing teeth remain equal. Therefore, the index does not improve with the treatment of caries. Additionally, it cannot be used to assess the prevalence of root caries in elderly individuals. CPI involves a labor-intensive and time-consuming process of individually probing the periodontal tissue around representative teeth using periodontal probing.
To overcome these disease-centered limitations of indicators, there has been a consistent proposal for evaluating oral health status using the number of present teeth or the number of functioning teeth, which aids in mastication [9]. Tooth loss is a key factor affecting the reduction of masticatory function, making the monitoring of present teeth a valuable indicator for assessing normal oral function. Aida et al (2011) [10] were the first to report the correlation between the number of teeth present and functional disability in a 6-year longitudinal study of 4,425 Japanese elderly aged over 65 years. The findings revealed that elders with fewer than 19 remaining teeth had a 1.21 times higher incidence of functional disability compared with those with 20 or more teeth. Another study tracking 1,763 Japanese elders aged 65 for 3 years found that those with fewer than 20 teeth had a 2.5 times increased risk of falls [11]. Research comparing cumulative survival rates over 10 years between groups of 80-year-old Japanese with more than 20 teeth and those with fewer than 20 teeth showed significantly higher survival rates [12].
Japan has used the number of teeth present as an indicator capable of assessing masticatory function instead of relying solely on disease-centered indicators such as the DMFT or CPI. This approach has allowed for the accumulation of academic evidence clarifying the correlation between oral health indicators, such as the number of teeth present, and overall health indicators, including general health status and survival rates.
Ⅳ. Japan’s 8020 Campaign
In 1981, the WHO and Federation Dentists International established dental health goals for the year 2000. One of these goals was to ensure that at least 50% of the population could maintain 20 functional teeth on their own. Japan was the first country to implement this internationally agreed-upon goal through a campaign targeting the elderly population.
The Japanese Ministry of Health, Labour and Welfare, along with the Japan Dental Association, initiated the 8020 Campaign in 1989, with the objective of “retaining 20 of one’s teeth until the age of 80” [13]. The 8020 Campaign in Japan specifically emphasized the necessity for the elderly, especially those over 80, to maintain 20 present teeth to preserve normal masticatory function, offering a clear quantitative goal rather than a vague qualitative slogan. The age of 80 was chosen as the core target age because it represents a transition point where independent activities decrease and dependency increases, entering the advanced age stage. Defining the minimum number of teeth necessary for adequate chewing as 20 and making this campaign’s central slogan was a significant endeavor.
In 1991, the Ministry allocated a budget of 7.57 million yen to establish adult dental health promotion councils in 10 regions, aiming to expand the 8020 campaign over the next 5 years as a pilot project. By 2000, the Ministry had significantly increased the budget to 580 million yen, launching a special 8020 campaign project to be conducted by prefectures that received strong support from the Japan Dental Association, leading to the campaign’s stabilization and expansion [13].
At the outset of the campaign in 1989, only 7% of Japanese elderly had achieved the 8020 goal, with an average of only four to five remaining teeth. However, as the campaign continued, the percentage of achievers rose to 10.9% in 1993, 24.1% in 2005, and 38.3% in 2011, exceeding 50% (51.6%) by 2016. Additionally, when examining the status of having 20 teeth among elderly individuals aged 75~79, who are nearing the age of 80, there has been a drastic improvement, from 10.0% in 1993 to 27.1% in 2005, and reaching 55.8% by 2022. Particularly noteworthy is the substantial increase in the number of individuals with 20 or more teeth from 1993 to 2022, especially in the 65~74 age group.
Thirty-five years have passed since the inception of the 8020 campaign in 1989, allowing for a comparison of its long-term cumulative effects. Thirty years before the start of the 8020 campaign in 1959, a person who was 20 years old would have lost an average of six teeth by the time they turned 50. However, for someone who was 20 in 1989 when the 8020 campaign began, the number of lost teeth reduced to 1.5 by the time they reached 50, which is only 25% of the teeth lost previously [14].
By 2016, the proportion of 80-year-old Japanese elders who had achieved the 8020 goal reached 51.6%, surpassing the initial target of 50%. Consequently, in 2018, the 8020 goal was revised from 50% to 60%. Following this, the Japanese Society of Oral Health proposed a new goal in place of the original 8020 Campaign, aiming for “28 teeth for a lifetime” [15].
Ⅴ. Impact of the 8020 Campaign: Effect on Oral and General Health
Risk factors that induce oral diseases share commonalities with those of chronic diseases, such as diabetes and hypertension. Therefore, behaviors that promote oral health are highly correlated with improvements in systemic health. This correlation has prompted numerous studies comparing various general health indicators between achievers and non-achievers of the 8020 Campaign post-implementation.
Iwasaki et al. (2019) [16] conducted a cohort study tracking individuals who had more than 20 teeth at the age of 70 for 10 years. Among them, those who retained all 28 teeth by the age of 80 years saw their total mortality rate significantly reduced by half (adjusted hazard ratio = 0.50) compared with those who experienced tooth loss.
Hashimoto et al. (2009) [17] reported in a cross-sectional study comparing 8020 achievers (N=217) with non-achievers (N=104) that achievers exhibited significantly higher masticatory ability and grip strength. Notably, female achievers had significantly higher bone density than non-achievers, and male achievers scored higher on balance tests than their non-achievers.
The impact of achieving the 8020 goal on non-communicable diseases such as diabetes and hypertension presents an intriguing area of research. A cohort study of Japanese adults aged 20 years and older, comparing those with 20 or more natural teeth (N=5607) to those with fewer than 19 teeth (N=904), examined various chronic conditions (diabetes, stroke, cardiovascular diseases, cancer, hypertension, and hyperlipidemia). The study found a significant trend of reduced incidence rates of diabetes, stroke, cardiovascular diseases, hypertension, and hyperlipidemia among adults with > 20 teeth [18].
Research by Kanda et al. (2008) [19] revealed that individuals with fewer teeth incurred significantly higher annual medical expenses in a cohort of 39,861 individuals who received medical and dental treatments over 3 years in 2002.
Furthermore, comprehensive and objective evaluations of the 8020 Campaign were conducted over the past three decades. Takehara et al (2023) [20] conducted a systematic review based on PRISMA guidelines, selecting 25 papers related to the 8020 campaign. Among these studies, some were financially supported by the 8020 Foundation, while a few lacked a clear explanation of the direct relationship with the 8020 campaign. Consequently, researchers argued for a more systematic explanation based on information about the campaign’s structure and activities to clearly demonstrate the direct link between Japan’s oral health improvements and the 8020 campaign over the past 30 years.
Ⅵ. Changes in Oral Health Behaviors After the 8020 Campaign
Since its inception by the Japanese government and the Japan Dental Association in 1989, the 8020 campaign has significantly influenced the Japanese public awareness of oral health over 35 years. Notably, the percentage of people brushing their teeth more than three times a day has more than doubled compared with 35 years ago. In 2022, 50.9% of the population used dental floss or interdental brushes, and 58% visited a dental clinic in the past year.
Significant social change has been observed in the market share of fluoride toothpaste. In 1988, the fluoride toothpaste held only a 30% market share in Japan. However, by 2002, it had significantly increased to 86%, and by 2020, it had expanded to 92%. Following this change, toothpaste with a fluoride concentration of 1450 ppm, in alignment with international standards, began to be sold in the Japanese market. In addition, changes in sugar consumption have been observed to affect dental caries. Annual sugar consumption per capita by Japanese people peaked at 30.4 kg in 1974, gradually decreasing to 15.3 kg by 2021 [21,22].
Ⅶ. Comparison of Oral Health Status Between Elderly in Korea and Japan
The first step in applying Japan’s successful experience with the 8020 Campaign to Korea is to conduct an epidemiological comparison of representative national statistics on oral health indicators between the two countries to understand past and present situations accurately.
The first direct comparison of oral health status between Korean and Japanese adults was published by Kim et al (2005) [23] This study used percentile curves, commonly employed for the growth and development curves of infants, to compare the number of present and healthy teeth among adults in both countries. The comparison was based on Japan’s 1999 (平成 11th year) Dental Disease Status Survey and Korea’s 2000 National Oral Health Survey, representing significant national statistics for adults aged 20~74. Our results showed that Korean adults had significantly lower rates of dental caries and a higher number of teeth present compared to the Japanese elderly. Japan has conducted national surveys on dental health since 1953 (昭和 32nd year), while Korea initiated its first National Oral Health Survey in 2000. Since 2007, oral examinations have been included in the 4th Korea National Health and Nutrition Examination Survey, providing national representative health statistics [24]. However, in Korea’s survey, participants aged over 80 years were grouped together, making it impossible to extract data specifically for those aged 80 years, unlike Japan’s national statistics. Considering these limitations, it was deemed realistic to compare the elderly aged 75~79 (late 70s), approaching 80 years, between Korea and Japan using post-2000 data, coinciding with Korea’s initiation of its national oral health survey.
A comparison of the proportion of elderly aged 75~79 with 20 or more teeth was conducted between the two countries. In 1999, 17.5% of Japanese elderly in this age group had 20 or more teeth, whereas in Korea, the figure was 30.4% (2000), making it 1.74 times higher. However, by 2005, while the figure for the Japanese elderly had improved significantly to 27.1%, the figure for the Korean elderly showed little change at 30.9% (2006), narrowing the gap between the two countries. By 2011, the proportion of Japanese elderly with 20 or more teeth had increased to 47.6%, but in Korea, it remained at 32.7%, marking the first time the figures reversed in favor of Japan. By 2016, the Japanese elderly surpassed the 50% mark for the first time, reaching 56.1%, whereas the Korean elderly accounted for 46.8% (2015). The most recent data from 2022 show that 55.8% of Japanese elderly had 20 or more teeth, and for the first time, Korea surpassed the 50% threshold, reaching 53.9% (2019) (Fig. 1).
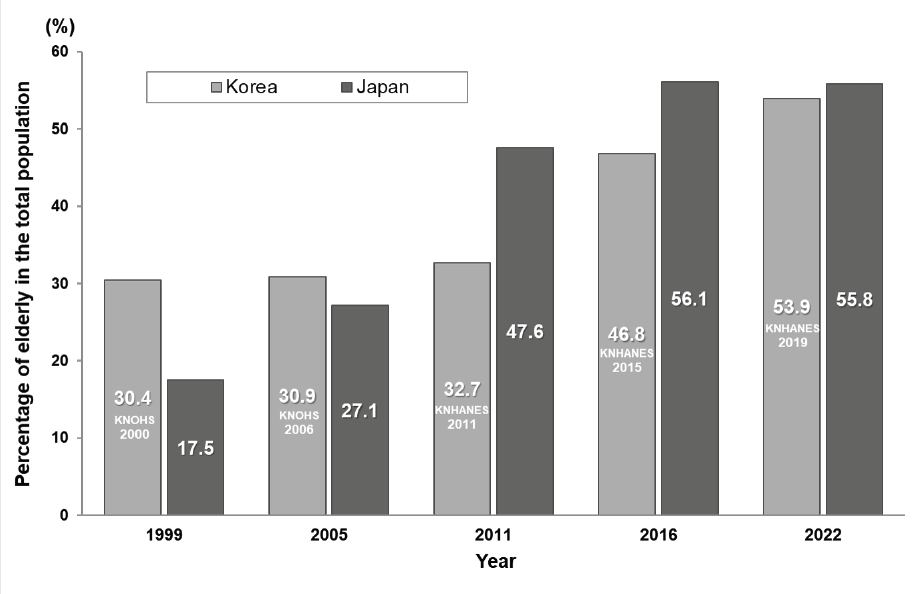
Changes in the proportion of elderly (aged 75–79) in Korea and Japan with 20 or more present teeth from 1999 to 2022. The numbers in the bar graph of Korea are the survey years. Data source: Japan Dental Diseases Survey (1999-2022); Korea National Oral Health Survey (2000-2006); Korea National Health and Nutrition Examination Survey (2010-2019)
A comparison of the average number of teeth in elderly individuals aged 75~79 in both countries yielded another significant result. In 1999, Japanese elders aged 75~79 had an average of 9.0 present teeth, whereas Korean elders had 13.1 teeth in 2000, possessing 4.1 more teeth than their Japanese counterparts [25]. By 2005, the gap had narrowed, with Japanese elders having 10.7 teeth and Koreans 13.5 teeth (2006). However, by 2011, Japanese elders saw a significant increase to 15.6 teeth, whereas Korean elders remained stagnant at 13.5 teeth, marking the first time that these figures had reversed. In 2016, the gap widened further, with Japanese elders having 18.0 teeth compared to 15.4 of Koreans (2015). The most recent data from 2022 show that Japanese elders have 18.1 teeth and Koreans have 17.6 teeth (2019), closing the gap between the two (Fig. 2).
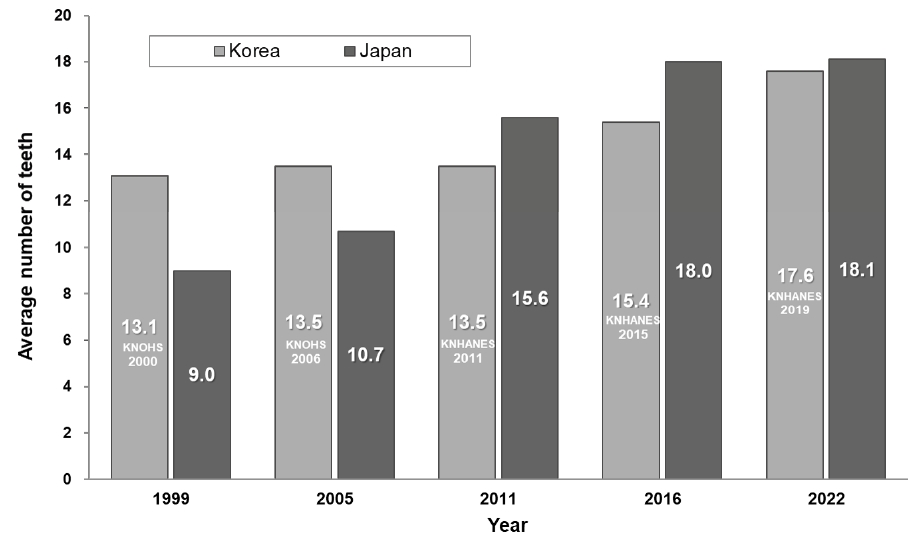
Changes in the average number of present teeth among the elderly (aged 75–79) in Korea and Japan from 1999 to 2022. The numbers in the bar graph of Korea are the survey years. Data source: Japan Dental Diseases Survey (1999-2022); Korea National Oral Health Survey (2000-2006); Korea National Health and Nutrition Examination Survey (2010-2019)
A comparison of the oral health of the elderly aged 75~79 in Korea and Japan over 5 years revealed that before 2011, Korean elders exhibited better oral health than Japanese elders. However, starting in 2011, the situation reversed, with the tooth retention rate among Japanese elders aged 75~79 significantly improved, surpassing the figures in Korea. The year 2011 marks 22 years after the start of Japan’s 8020 campaign in 1989, suggesting that the outcomes of the campaign during this period became visibly evident.
Ⅷ. Conclusion
Traditionally, a generation has been defined as a period spanning 30 years. The 8020 campaign, initiated in Japan in 1989, has surpassed one generation and marked 35 years. The goal of maintaining 20 healthy natural teeth by the age of 80 was considered lofty at the campaign’s inception but challenging to achieve. However, as the campaign progressed, gradual changes emerged. Visible improvements in the number of individuals maintaining 20 or more teeth and the average number of teeth present were observed a decade after the project’s implementation. By 2011, 22 years after the campaign’s implementation, the oral health status of Japanese elders, previously inferior to that of Korean elders, had surpassed that of Koreans. With the 8020 campaign goals partially achieved, the Japanese dental community is now preparing new oral health objectives aimed at “preventing tooth loss throughout life in line with increases in life expectancy”. The successful outcomes of Japan’s 8020 campaign can be attributed to the concerted efforts of the Japanese central government, local governments, and the dental community in setting specific, achievable goals, with consistent financial support from the central government, and sustaining these efforts not just for a short term, but over a generation.
Korea implemented pioneering oral health policies ahead of Japan, such as the Water Fluoridation Project in 1981 and the enactment of the Oral Health Act in 2000. Water fluoridation projects became the cornerstone of Korea’s oral health initiatives. However, after expanding to cover 9.4% of the population in 2001, 20 years after its inception, the project rapidly declined, and by 2018, 38 years after its launch, all water fluoridation projects were discontinued [26]. Since then, Korea’s oral health sector has largely focused on sporadic oral health initiatives led by local governments without clear overarching goals.
Now, Korea also needs to set specific and ambitious goals comparable to Japan's 8020 Campaign through in-depth discussions between the central government and the dental community. To achieve this, the following measures need to be concretely implemented:
First, it is necessary to create a core slogan that reflects the Korean context, similar to Japan's “8020 Campaign”. This involves comprehensively considering Korea's demographic structure, oral health status, and setting clear and achievable goals over the next decade. These goals should be easily understood by the public to encourage interest and participation in oral health. The goal-setting process should involve dental experts, health policy experts, and the general public to establish more realistic and achievable objectives.
Second, there is a need for continuous financial support and the establishment of a dedicated organization to focus on these initiatives. The continuous financial support from the Japanese government significantly contributed to the success of the campaign, and this is also essential for Korea. The central government should secure long-term funding to support various programs aimed at improving oral health. Additionally, a dedicated organization should be formed to systematically and effectively implement these initiatives. This organization should coordinate cooperation between the central and local governments and develop specific implementation plans.
Third, policy support and research foundations must be strengthened. It is necessary to expand research related to oral health to formulate policies based on scientific evidence. The government, academia, and the dental community should collaborate to conduct research and reflect the findings in policies. This approach will help obtain more accurate data and information on oral health, which can be used to develop efficient and effective policies.
Lastly, the success of Japan's 8020 Campaign was due to sustained efforts over more than 30 years. Therefore, Korea should not expect short-term results but instead implement long-term financial support and sustainable policies for at least one generation. If these efforts are consistently maintained, the oral health of Korean elderly can be significantly improved.
The significance of this study lies in systematically reviewing and introducing Japan's 8020 Campaign, which has not been widely known in Korea. Additionally, it is the first to compare the oral health status of elderly individuals in Korea and Japan using the number of present teeth, a measure closely related to systemic health and healthy lifespan. This study can serve as an important reference for Korea to benchmark Japan's successful example and make concrete and sustained efforts to improve oral health.
The limitations of this study include the inability to obtain primary data from Japan, resulting in a comparison based on secondary data from reports and processed Korean data. Moreover, the study did not quantitatively evaluate and present the impact of the 8020 Campaign on the improvement of oral health in Japan. To address these limitations, future research should use more comparable time-series data and conduct comparative studies that consider cultural and social differences.
Ⅸ. Conflicts of Interest
The authors declare no conflict of interest.
